Barrett’s esophagus is a condition where the normal squamous epithelium lining of the esophagus transforms into specialized intestinal metaplasia due to chronic gastroesophageal reflux disease (GERD). This transformation increases the risk of dysplasia, which can progress to esophageal adenocarcinoma.
High-grade dysplasia (HGD) is considered a precancerous stage where abnormal cells exhibit significant structural disorganization and an increased risk of progression to invasive cancer.
Causes and Risk Factors of High-Grade Dysplasia
Several factors contribute to the development of high-grade dysplasia in Barrett’s esophagus, including:
- Chronic GERD: Long-term acid reflux damages the esophageal lining.
- Genetic Predisposition: Family history of Barrett’s esophagus and esophageal cancer increases risk.
- Tobacco and Alcohol Use: Both are linked to cellular damage and increased dysplasia risk.
- Obesity: Particularly central obesity, which increases intra-abdominal pressure, leading to more severe reflux.
- Dietary Factors: Low intake of fruits and vegetables, high consumption of processed and red meats.
Diagnosis of High-Grade Dysplasia
Diagnosis requires a combination of endoscopic evaluation and histological analysis. The key diagnostic methods include:
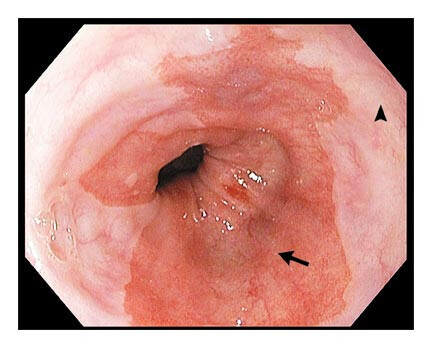
Endoscopy with Biopsy
Upper endoscopy is performed to visually inspect the esophageal lining and obtain biopsy samples for histopathological examination.
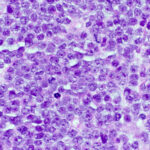
Histological Assessment
A pathologist examines the biopsy under a microscope to identify cellular abnormalities characteristic of HGD, such as:
- Loss of normal cell polarity
- Increased nuclear-to-cytoplasmic ratio
- Mitoses and architectural distortion
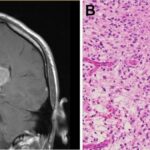
Endoscopic Ultrasound (EUS)
EUS helps assess the depth of dysplastic changes and detect early signs of invasive carcinoma.
Molecular Markers and Biomarkers
Emerging diagnostic tools include p53 immunohistochemistry and DNA content abnormalities, which help in risk stratification.
Treatment Options for High-Grade Dysplasia
Given the high risk of progression to esophageal adenocarcinoma, treatment is strongly recommended. Available options include:
Endoscopic Resection (ER)
Endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) can remove dysplastic lesions and provide a definitive histological diagnosis.
Radiofrequency Ablation (RFA)
RFA uses heat energy to destroy dysplastic tissue and is often performed after EMR to eliminate residual abnormal cells.
Cryotherapy
This method freezes and destroys abnormal cells in the esophageal lining, offering an alternative for patients unsuitable for RFA.
Photodynamic Therapy (PDT)
PDT involves administering a photosensitizing agent followed by light activation to target dysplastic tissue.
Esophagectomy
For patients with multifocal HGD or non-responsive dysplasia, esophagectomy (surgical removal of the esophagus) may be considered, particularly if there is a concern for occult cancer.
Surveillance and Follow-Up
Patients with Barrett’s esophagus and a history of HGD require regular monitoring through endoscopic surveillance to detect recurrence. Recommended intervals for endoscopic evaluation are:
- Every 3–6 months for patients undergoing non-surgical treatment.
- Annually for patients with complete eradication of dysplasia post-treatment.
Prognosis and Cancer Risk
Without intervention, up to 30–50% of patients with HGD progress to esophageal adenocarcinoma within five years. Early detection and appropriate treatment significantly reduce cancer risk and improve long-term outcomes.
High-grade dysplasia in Barrett’s esophagus represents a critical stage in the development of esophageal adenocarcinoma. Early detection through endoscopic surveillance and timely intervention using advanced endoscopic therapies or surgical approaches significantly improves patient outcomes. Individuals with Barrett’s esophagus should undergo regular monitoring to ensure early diagnosis and optimal treatment.