Hereditary Tyrosinemia Type I (HT1) is a rare genetic disorder caused by a deficiency in the enzyme fumarylacetoacetate hydrolase (FAH). This enzyme is essential in the breakdown of the amino acid tyrosine. The absence of FAH leads to the accumulation of toxic metabolites in the liver and kidneys, resulting in severe complications.

Causes of Hereditary Tyrosinemia Type I
HT1 is an autosomal recessive disorder, meaning both parents must carry the defective gene for their child to develop the condition. The FAH gene mutation leads to insufficient FAH enzyme production, resulting in the toxic buildup of substances like succinylacetone, which impairs cellular function.
Symptoms of Hereditary Tyrosinemia Type I
Symptoms may vary but typically manifest in early infancy. Common symptoms include:
- Failure to thrive
- Jaundice
- Hepatomegaly (enlarged liver)
- Vomiting and diarrhea
- Peripheral neuropathy
- Renal dysfunction
- Increased risk of liver cancer
Diagnosis of Hereditary Tyrosinemia Type I
Early diagnosis is critical to manage the condition effectively. Diagnostic methods include:
- Newborn Screening: Detects elevated levels of succinylacetone in blood.
- Blood and Urine Tests: Measure tyrosine and metabolite levels.
- Genetic Testing: Identifies mutations in the FAH gene.
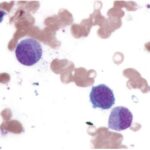
- Liver Biopsy: Conducted in unclear cases to assess liver damage.
Treatment Options for Hereditary Tyrosinemia Type I
Treatment strategies aim to reduce toxic metabolite accumulation and improve quality of life.
1. Nitisinone (NTBC) Therapy
- Nitisinone inhibits the enzyme 4-hydroxyphenylpyruvate dioxygenase, reducing toxic byproducts.
- Regular monitoring is essential to manage tyrosine levels.
2. Dietary Management
- A low-tyrosine and low-phenylalanine diet is crucial.
- Patients should consume specialized formulas under medical supervision.
3. Liver Transplant
- In severe cases where medical treatment fails, a liver transplant may be the only viable option.
Prognosis and Life Expectancy
With early diagnosis and proper treatment, individuals with HT1 can lead relatively normal lives. Delayed treatment significantly increases the risk of liver failure and hepatocellular carcinoma.
Prevention and Genetic Counseling
Genetic counseling is strongly recommended for families with a history of HT1. Carrier screening can help identify individuals at risk of transmitting the disorder.
FAQs
1. What is the life expectancy of someone with HT1?
With appropriate treatment, individuals diagnosed early can achieve a normal lifespan.
2. Can HT1 be cured?
While Nitisinone and dietary management control symptoms, liver transplant remains the only definitive cure.
3. How common is hereditary tyrosinemia type I?
HT1 is rare, with an estimated incidence of 1 in 100,000 births worldwide.
4. What foods should patients with HT1 avoid?
Patients should avoid protein-rich foods such as meat, eggs, and dairy to manage tyrosine levels effectively.
5. Is hereditary tyrosinemia type I detected at birth?
Yes, newborn screening programs in many countries include HT1 testing to enable early diagnosis and intervention.