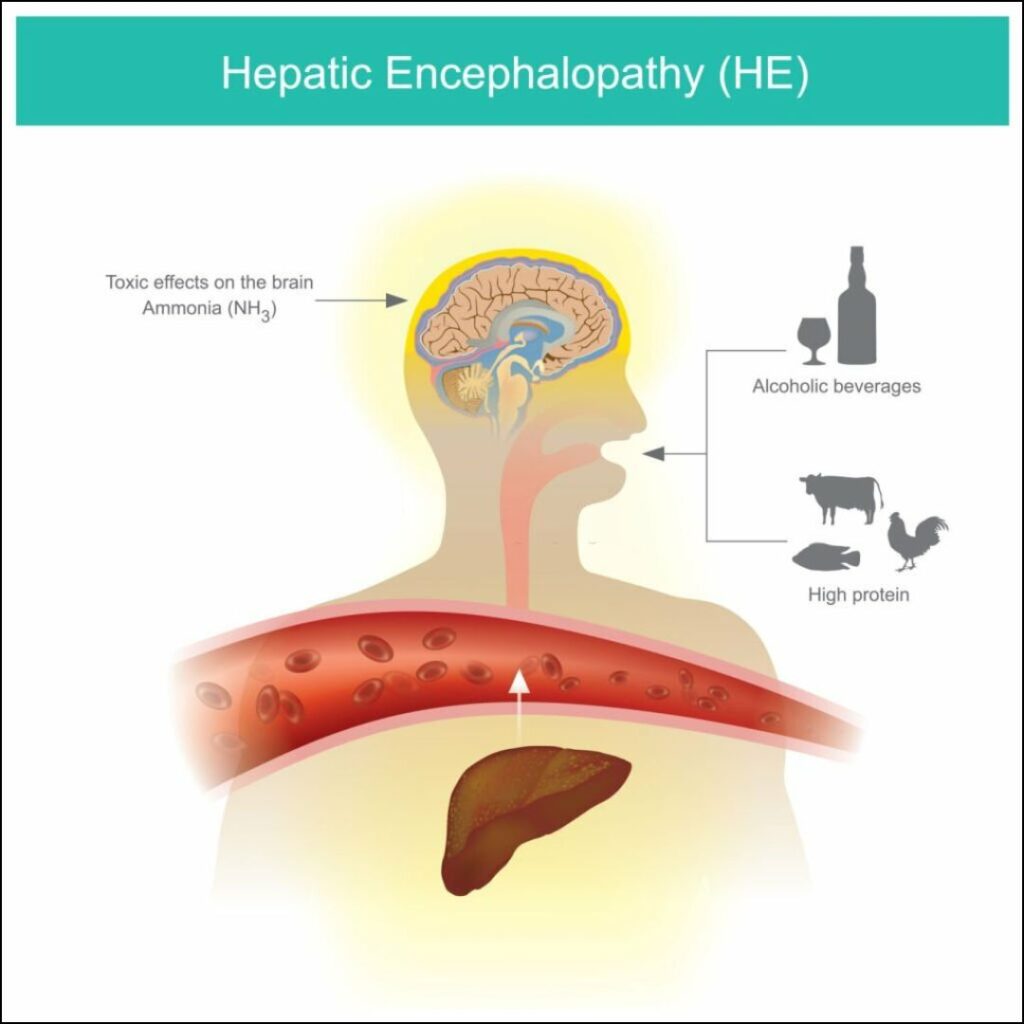
Hepatic encephalopathy (HE) is a complex neurological disorder resulting from liver dysfunction, primarily seen in patients with chronic liver disease or acute liver failure. This condition arises due to the accumulation of toxic substances in the bloodstream that the liver fails to adequately filter. HE can present in various forms, ranging from mild cognitive impairment to coma, making prompt diagnosis and treatment essential.
Causes of Hepatic Encephalopathy
Hepatic encephalopathy is primarily associated with liver-related conditions that impair the organ’s ability to detoxify the bloodstream. Common causes include:
- Cirrhosis: The most frequent cause, often linked to alcohol abuse, hepatitis, or fatty liver disease.
- Acute Liver Failure: A sudden and severe impairment of liver function.
- Portosystemic Shunting: Abnormal blood flow bypassing the liver, allowing toxins to accumulate.
- Gastrointestinal Bleeding: Increases nitrogenous waste in the blood, triggering HE.
- Infections: Can worsen pre-existing liver conditions, inducing HE.
- Electrolyte Imbalances: Particularly low sodium or potassium levels.
- Medications: Certain drugs like sedatives or tranquilizers may exacerbate HE symptoms.
Symptoms of Hepatic Encephalopathy
The symptoms of HE can vary significantly depending on its severity. These are categorized into four stages:
- Stage 1 (Mild): Mood changes, confusion, mild memory loss, or sleep disturbances.
- Stage 2 (Moderate): Lethargy, personality changes, and disorientation.
- Stage 3 (Severe): Marked confusion, bizarre behavior, and extreme drowsiness.
- Stage 4 (Coma): Unresponsiveness requiring immediate medical intervention.
Other symptoms may include tremors, slurred speech, muscle stiffness, and a distinctive musty odor on the breath.
Diagnosis of Hepatic Encephalopathy
Diagnosing HE requires a combination of clinical evaluation and diagnostic tests:
- Medical History and Physical Examination: Assessing risk factors such as liver disease history.
- Blood Tests: Evaluating ammonia levels, liver function tests (LFTs), and electrolyte imbalances.
- Neuropsychological Testing: Identifying cognitive impairments.
- Imaging Tests: MRI or CT scans to rule out other neurological disorders.
Treatment Options for Hepatic Encephalopathy
Treatment strategies aim to reduce toxins in the bloodstream and manage underlying liver conditions. Common approaches include:
- Lactulose: A non-absorbable sugar that reduces ammonia absorption in the intestines.
- Rifaximin: An antibiotic that decreases ammonia-producing gut bacteria.
- Probiotics: May improve gut health and reduce toxin buildup.
- Dietary Management: Controlled protein intake to balance ammonia production and nutrient requirements.
- Liver Transplant: Recommended for patients with end-stage liver disease when other treatments prove ineffective.
Preventive Measures for Hepatic Encephalopathy
To reduce the risk of developing HE, patients with liver conditions should:
- Follow prescribed medications and treatment plans.
- Avoid alcohol and hepatotoxic drugs.
- Maintain a balanced diet, rich in fruits, vegetables, and lean proteins.
- Manage co-existing conditions such as diabetes or hypertension.
Prognosis and Long-Term Outlook
The prognosis for hepatic encephalopathy varies based on its underlying cause, severity, and response to treatment. Early-stage HE typically has a favorable outlook with proper management, while advanced HE may require long-term care or liver transplantation.
Frequently Asked Questions
Q1: Is hepatic encephalopathy reversible?
A: Yes, in its early stages, hepatic encephalopathy is often reversible with appropriate treatment and lifestyle adjustments.
Q2: Can hepatic encephalopathy recur?
A: Yes, recurrence is possible if underlying liver conditions remain unmanaged.
Q3: What are common triggers for hepatic encephalopathy?
A: Triggers include gastrointestinal bleeding, infections, constipation, dehydration, and certain medications.
Q4: How is hepatic encephalopathy different from other neurological conditions?
A: HE is unique as its symptoms are directly linked to liver dysfunction, and treatment focuses on reducing toxins in the bloodstream.
Q5: Can diet help manage hepatic encephalopathy?
A: Yes, a well-balanced diet with controlled protein intake can support recovery and prevent episodes.
Hepatic encephalopathy is a serious yet manageable condition with prompt diagnosis and appropriate intervention. Understanding its causes, symptoms, and treatments is crucial for improving patient outcomes. Regular medical follow-up and adherence to prescribed therapies are essential to managing this condition effectively.