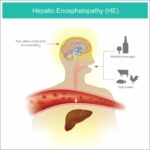
Hepatic coma, also known as stage 4 hepatic encephalopathy, is a severe and life-threatening condition resulting from liver failure. It occurs when toxins such as ammonia accumulate in the bloodstream, impairing brain function. This condition requires immediate medical intervention to prevent fatal outcomes.
Causes of Hepatic Coma
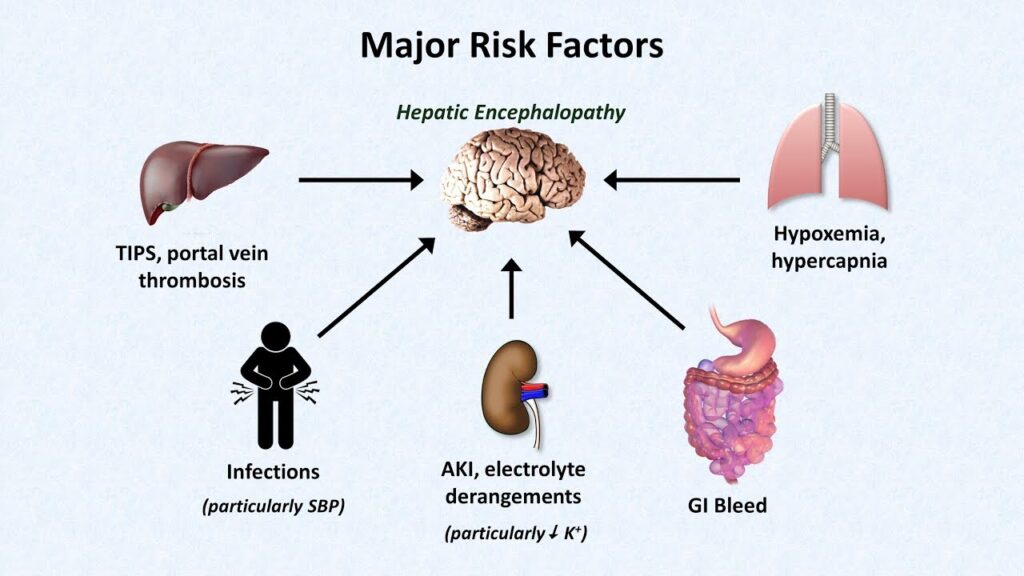
Several factors can trigger hepatic coma, including:
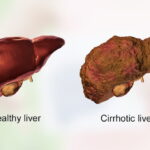
- Chronic Liver Disease: Conditions like cirrhosis and hepatitis.
- Alcohol Abuse: Long-term alcohol consumption damaging liver cells.
- Drug Overdose: Certain medications, especially sedatives and opioids.
- Gastrointestinal Bleeding: Increases nitrogenous waste absorption.
- Infections: Trigger inflammatory responses that impair liver function.
- Electrolyte Imbalance: Especially low potassium levels.
Stages of Hepatic Encephalopathy
Hepatic encephalopathy progresses through four stages:
- Stage 1: Mild confusion, personality changes, and mood swings.
- Stage 2: Lethargy, disorientation, and tremors.
- Stage 3: Severe confusion, inappropriate behavior, and incoherent speech.
- Stage 4 (Hepatic Coma): Unresponsiveness with potential risk of death.
Symptoms of Hepatic Coma
- Severe confusion and disorientation
- Extreme drowsiness or unresponsiveness
- Jaundice (yellowing of skin and eyes)
- Breath with a musty or sweet odor
- Tremors and muscle stiffness
- Seizures and unconsciousness in severe cases
Diagnosis of Hepatic Coma
Medical professionals use the following methods to diagnose hepatic coma:
- Blood Tests: Check ammonia levels, liver enzymes, and electrolyte balance.
- Imaging Tests: MRI or CT scans to assess brain swelling.
- Electroencephalogram (EEG): Detects abnormal brain activity.
- Neurological Exams: Assess cognitive function and reflexes.
Treatment for Hepatic Coma
Treatment aims to manage the underlying cause and reduce toxin buildup:
1. Medication
- Lactulose: Reduces ammonia absorption in the intestines.
- Rifaximin: Controls bacterial overgrowth in the gut.
- Neomycin or Metronidazole: Used in severe bacterial imbalances.
2. Dietary Changes
- Reduce protein intake to minimize ammonia production.
- Increase fiber to promote regular bowel movements.
3. Liver Support and Transplant
- For patients with severe liver damage, a liver transplant may be the only viable option.
Prevention Strategies
Preventing hepatic coma involves proactive liver health management:
- Avoid excessive alcohol consumption.
- Maintain a balanced diet and healthy weight.
- Follow prescribed treatments for chronic liver conditions.
- Schedule regular medical check-ups to monitor liver function.
Prognosis and Recovery
Early diagnosis and prompt treatment significantly improve recovery chances. However, delayed intervention can result in permanent brain damage or death. Patients with chronic liver conditions should adhere to medical advice and lifestyle changes to prevent hepatic coma recurrence.
Frequently Asked Questions
What is the primary cause of hepatic coma?
Hepatic coma is commonly caused by chronic liver diseases such as cirrhosis and hepatitis, compounded by ammonia buildup in the bloodstream.
How is hepatic coma treated in emergencies?
Emergency treatment includes administering lactulose, intravenous fluids, and antibiotics while stabilizing the patient’s vital functions.
Can hepatic coma be reversed?
If diagnosed early, hepatic coma can be managed and even reversed with appropriate medical intervention and lifestyle adjustments.
Is hepatic coma fatal?
Without prompt treatment, hepatic coma can be fatal. Early diagnosis and effective treatment improve survival rates significantly.
How can one reduce the risk of hepatic coma?
Maintaining liver health through a balanced diet, limiting alcohol intake, and treating underlying liver conditions can help prevent hepatic coma.