Haemophilus parainfluenzae pneumonia is a rare but significant bacterial respiratory infection caused by Haemophilus parainfluenzae, a member of the normal flora of the upper respiratory tract. Although typically commensal, this bacterium can become pathogenic under certain conditions, leading to pneumonia. Early diagnosis and appropriate treatment are crucial for optimal patient outcomes.
Understanding Haemophilus Parainfluenzae
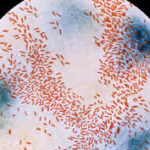
Haemophilus parainfluenzae is a gram-negative, facultative anaerobic coccobacillus. It belongs to the Pasteurellaceae family and is commonly found in the human nasopharynx. Although less virulent than Haemophilus influenzae, it can cause opportunistic infections, particularly in immunocompromised individuals or those with underlying health conditions.
Pathogenesis
The pathogenesis of Haemophilus parainfluenzae pneumonia involves bacterial colonization of the respiratory tract, followed by invasion and inflammation in the lower airways. Factors that increase susceptibility include:
- Chronic obstructive pulmonary disease (COPD)
- Immunosuppression
- Recent respiratory viral infection
- Aspiration of oropharyngeal secretions
- Smoking and environmental pollutants
Clinical Presentation
Symptoms of Haemophilus parainfluenzae pneumonia closely resemble other bacterial pneumonias. Patients may present with:
- Cough (productive or dry)
- Fever and chills
- Shortness of breath (dyspnea)
- Chest pain (pleuritic in nature)
- Fatigue and malaise
- Purulent sputum production
In severe cases, patients may experience respiratory distress, hypoxia, and signs of systemic infection, necessitating urgent medical intervention.
Diagnosis of Haemophilus Parainfluenzae Pneumonia
Accurate diagnosis requires a combination of clinical evaluation and laboratory testing. Key diagnostic methods include:
1. Clinical Assessment
- Detailed patient history (e.g., recent illnesses, immunosuppressive conditions)
- Physical examination (crackles, decreased breath sounds, signs of consolidation)
2. Microbiological Testing
- Sputum Gram stain and culture (revealing gram-negative coccobacilli)
- Blood cultures in cases of suspected bacteremia
- Polymerase chain reaction (PCR) for enhanced sensitivity
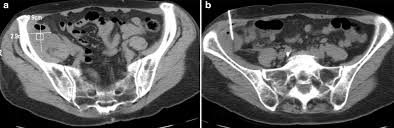
3. Imaging Studies
- Chest X-ray: Revealing lobar or bronchopneumonia patterns
- Computed Tomography (CT) scan: Useful for identifying abscesses or pleural effusions
Treatment Strategies
Management of Haemophilus parainfluenzae pneumonia typically involves antimicrobial therapy tailored to bacterial susceptibility. First-line treatments include:
1. Antibiotic Therapy
- Beta-lactam antibiotics (e.g., amoxicillin-clavulanate)
- Third-generation cephalosporins (e.g., ceftriaxone)
- Fluoroquinolones (e.g., levofloxacin) for penicillin-allergic patients
2. Supportive Care
- Oxygen therapy for hypoxia
- Intravenous fluids to maintain hydration
- Antipyretics for fever management
3. Monitoring and Follow-up
- Regular assessment of clinical symptoms
- Repeat imaging in persistent cases
Prevention and Risk Reduction
Preventative measures focus on reducing exposure and strengthening host defenses:
- Vaccination: While no specific vaccine targets H. parainfluenzae, routine influenza and pneumococcal vaccines lower co-infection risks.
- Infection Control: Hand hygiene and respiratory precautions in healthcare settings.
- Chronic Disease Management: Optimizing control of comorbidities (e.g., diabetes, COPD).
Prognosis and Complications
With prompt antibiotic therapy, the prognosis for Haemophilus parainfluenzae pneumonia is generally favorable. However, delayed treatment or underlying health issues may lead to complications, including:
- Lung abscess
- Pleural effusion
- Respiratory failure
- Sepsis
Haemophilus parainfluenzae pneumonia is a potentially serious infection requiring early recognition and effective antimicrobial management. Clinicians must maintain vigilance, particularly in high-risk patients, to ensure timely diagnosis and optimal outcomes. Ongoing research may further elucidate the pathogen’s behavior and improve therapeutic strategies.