Haemophilus influenzae lung abscess is a rare but severe pulmonary condition caused by the bacterial pathogen Haemophilus influenzae. This infection can result in the formation of localized pus-filled cavities within the lung tissue. Early identification and treatment are critical to prevent life-threatening complications and ensure optimal patient outcomes.

Understanding Haemophilus Influenzae
Haemophilus influenzae is a gram-negative, facultative anaerobic bacterium that resides in the upper respiratory tract. Although it is often associated with otitis media, sinusitis, and meningitis, it can also lead to severe pulmonary infections, particularly in immunocompromised individuals.
Pathophysiology of Haemophilus Influenzae Lung Abscess
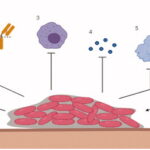
Lung abscesses develop when bacteria infiltrate lung tissue, causing inflammation and necrosis. Haemophilus influenzae typically enters the lungs via aspiration or hematogenous spread, leading to localized infection. As the immune response activates, a cavity filled with pus forms within the lung parenchyma.
Causes and Risk Factors
Several factors increase the likelihood of developing a Haemophilus influenzae lung abscess, including:
- Aspiration of Oral Secretions: Common in patients with reduced consciousness due to anesthesia, alcohol intoxication, or neurological conditions.
- Immunosuppression: Individuals with compromised immune systems (e.g., from chemotherapy, HIV, or corticosteroid use) are at higher risk.
- Chronic Pulmonary Disease: Conditions such as chronic obstructive pulmonary disease (COPD) and bronchiectasis predispose patients to lung infections.
- Recent Respiratory Infections: Viral illnesses can facilitate bacterial superinfection and abscess formation.
- Dental Infections: Poor oral hygiene and dental abscesses may introduce pathogens through aspiration.
Clinical Presentation
Symptoms of Haemophilus influenzae lung abscess are often non-specific but may include:
- Persistent cough with purulent or foul-smelling sputum
- Fever, chills, and night sweats
- Pleuritic chest pain
- Dyspnea (shortness of breath)
- Weight loss and fatigue
- Hemoptysis (coughing up blood) in severe cases
Diagnostic Evaluation
Prompt and accurate diagnosis of Haemophilus influenzae lung abscess involves multiple clinical and imaging approaches.
Clinical Assessment
A thorough medical history and physical examination are essential. Patients often present with a prolonged history of respiratory symptoms and systemic signs of infection.
Imaging Studies
- Chest X-ray: Identifies cavitary lesions with air-fluid levels characteristic of lung abscesses.
- Computed Tomography (CT) Scan: Provides detailed visualization of the abscess, surrounding lung tissue, and potential complications.
Microbiological Testing
- Sputum Culture: Identifies Haemophilus influenzae and guides antibiotic therapy.
- Blood Cultures: Useful for detecting bacteremia in systemic infection.
- Bronchoscopy with Aspiration: Allows direct sampling of the infected site when non-invasive methods are inconclusive.
Treatment Strategies
Effective management of Haemophilus influenzae lung abscess combines antimicrobial therapy, supportive care, and, in some cases, surgical intervention.
Antibiotic Therapy
Empiric broad-spectrum antibiotics should be initiated promptly, with subsequent tailoring based on culture results. Recommended regimens include:
- Beta-lactam/Beta-lactamase Inhibitors: Such as ampicillin-sulbactam or piperacillin-tazobactam.
- Cephalosporins: Third-generation options like ceftriaxone are effective against Haemophilus influenzae.
- Combination Therapy: Consider adding metronidazole if anaerobic co-infection is suspected.
Duration of Therapy
A minimum of 4 to 6 weeks of antibiotic treatment is typically required, with adjustments based on clinical and radiological improvement.
Supportive Care
- Oxygen supplementation for hypoxemia
- Fluid management to prevent dehydration
- Nutritional support to aid recovery
Surgical Intervention
In cases of antibiotic failure, large abscesses, or persistent infection, surgical drainage or lobectomy may be necessary.
Prognosis and Complications
With timely diagnosis and appropriate treatment, the prognosis for Haemophilus influenzae lung abscess is generally favorable. Delayed intervention can lead to severe complications, including:
- Empyema (pus accumulation in the pleural cavity)
- Bronchopleural fistula
- Sepsis and multi-organ failure
- Chronic pulmonary fibrosis
Prevention Strategies
Preventing Haemophilus influenzae lung abscess involves addressing risk factors and promoting respiratory health:
- Vaccination: Ensure immunization with the Haemophilus influenzae type b (Hib) vaccine.
- Aspiration Precautions: Implement measures to prevent aspiration in at-risk patients.
- Oral Hygiene: Maintain proper dental care to reduce bacterial colonization.
- Management of Chronic Conditions: Control underlying respiratory diseases and immunosuppression.
Haemophilus influenzae lung abscess is a serious infectious condition requiring prompt diagnosis and comprehensive treatment. Understanding the pathophysiology, risk factors, and management strategies is essential for optimizing patient outcomes and preventing long-term complications. Early intervention remains the cornerstone of successful care and recovery.