Haemophilus influenzae chronic bronchitis is a persistent inflammatory condition of the bronchial tubes caused by infection with Haemophilus influenzae bacteria. This gram-negative bacterium is a common cause of respiratory tract infections, particularly in individuals with underlying lung conditions or compromised immune systems. Left untreated, it can lead to severe complications and a decline in respiratory function.
Causes of Haemophilus Influenzae Chronic Bronchitis
Chronic bronchitis caused by Haemophilus influenzae typically occurs when the bacterium colonizes the respiratory tract, triggering prolonged inflammation. Factors contributing to susceptibility include:
- Chronic Obstructive Pulmonary Disease (COPD): Patients with COPD are more prone to bacterial colonization due to impaired mucociliary clearance.
- Smoking: Damages respiratory defenses, making the bronchial mucosa more vulnerable.
- Weakened Immune System: Conditions like diabetes, HIV, and immunosuppressive therapy increase the risk.
- Environmental Exposure: Pollution and occupational hazards contribute to chronic airway irritation.
Symptoms of Haemophilus Influenzae Chronic Bronchitis
The clinical presentation of chronic bronchitis caused by Haemophilus influenzae includes both typical and atypical respiratory symptoms:
- Persistent productive cough with purulent sputum
- Shortness of breath (dyspnea)
- Wheezing and chest tightness
- Recurrent respiratory infections
- Fever and fatigue during exacerbations
Severe cases may lead to respiratory failure if not managed promptly.
Diagnosis of Haemophilus Influenzae Chronic Bronchitis
Accurate diagnosis involves a combination of clinical evaluation, microbiological testing, and imaging studies:
- Patient History and Physical Examination: Assessing symptom duration and risk factors.
- Sputum Culture and Gram Stain: Identifying Haemophilus influenzae through bacterial culture.
- Polymerase Chain Reaction (PCR): Detecting bacterial DNA for rapid identification.
- Chest X-Ray: Evaluating lung abnormalities and ruling out other conditions.
- Pulmonary Function Tests: Measuring airflow limitation and chronic bronchitis severity.
Treatment of Haemophilus Influenzae Chronic Bronchitis
Management focuses on eradicating the bacterial infection, reducing inflammation, and improving lung function.
Antibiotic Therapy
Effective antibiotic selection depends on bacterial resistance patterns:
- First-Line Antibiotics: Amoxicillin-clavulanate, second or third-generation cephalosporins
- Alternative Antibiotics: Fluoroquinolones (e.g., levofloxacin) for resistant strains
- Macrolides: For patients allergic to beta-lactam antibiotics
Supportive Care
Symptom management and patient support play a crucial role:
- Bronchodilators: Alleviate airway constriction
- Corticosteroids: Reduce inflammation during exacerbations
- Oxygen Therapy: For patients with hypoxemia
Monitoring and Follow-Up
Regular monitoring is essential to assess treatment efficacy and prevent recurrence:
- Repeat sputum cultures for persistent symptoms
- Pulmonary function tests to evaluate lung function
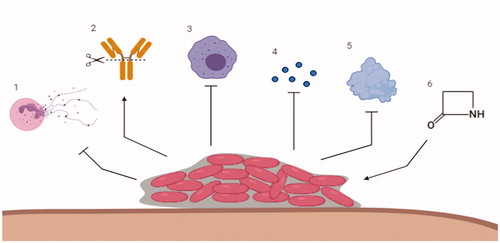
Prevention of Haemophilus Influenzae Chronic Bronchitis
Preventive strategies focus on reducing bacterial exposure and enhancing respiratory health:
- Vaccination: Annual influenza vaccine and pneumococcal immunization
- Smoking Cessation: Significantly lowers infection risk
- Infection Control: Hand hygiene and avoiding sick contacts
- Pulmonary Rehabilitation: Strengthens lung function in chronic patients
Prognosis and Long-Term Outlook
With prompt diagnosis and appropriate treatment, most patients achieve symptom relief and improved lung function. However, untreated or recurrent infections may lead to progressive airway damage and chronic respiratory failure. Comprehensive care and adherence to preventive measures enhance patient outcomes.
Haemophilus influenzae chronic bronchitis represents a significant cause of respiratory morbidity, particularly in vulnerable populations. Early identification, targeted antibiotic therapy, and preventive interventions are essential for effective management and improved patient quality of life.

