Haemophilus influenzae bronchitis is a bacterial infection of the bronchial tubes caused by the Haemophilus influenzae bacterium. This respiratory condition may lead to acute or chronic bronchitis, particularly in individuals with compromised immune systems, pre-existing lung disease, or those exposed to environmental risk factors. Timely diagnosis and appropriate antibiotic therapy are critical to managing and preventing complications.
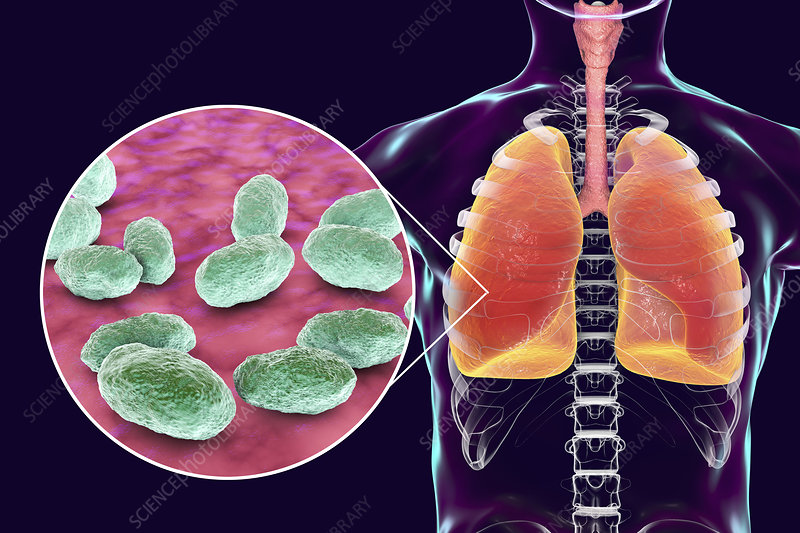
What is Haemophilus Influenzae?
Haemophilus influenzae is a Gram-negative, facultatively anaerobic bacterium that colonizes the upper respiratory tract. While non-typeable strains commonly cause bronchitis, type b (Hib) can lead to severe invasive diseases such as meningitis and pneumonia.
Key Characteristics of Haemophilus Influenzae
- Classification: Gram-negative coccobacillus
- Transmission: Respiratory droplets
- Types: Typeable (e.g., Hib) and non-typeable (NTHi)
- Pathogenicity: Opportunistic pathogen, especially in immunocompromised hosts
Causes and Risk Factors of Haemophilus Influenzae Bronchitis
Causes
Haemophilus influenzae bronchitis arises when the bacterium infects the bronchial mucosa, triggering inflammation and respiratory symptoms.
Risk Factors
- Age: Infants, elderly
- Chronic Conditions: Chronic obstructive pulmonary disease (COPD), asthma
- Smoking: Damages bronchial epithelium
- Immunosuppression: Chemotherapy, HIV
- Environmental Exposure: Air pollution, occupational hazards
Symptoms of Haemophilus Influenzae Bronchitis
Symptoms range from mild to severe and may overlap with other respiratory infections. Prompt recognition is essential for accurate diagnosis and treatment.
Common Symptoms
- Persistent cough with mucus (productive cough)
- Shortness of breath (dyspnea)
- Chest discomfort
- Fever and chills
- Fatigue and malaise
Diagnosis of Haemophilus Influenzae Bronchitis
Accurate diagnosis involves a combination of clinical evaluation, microbiological testing, and imaging studies.
Diagnostic Methods
- Clinical Assessment: Evaluation of symptoms and medical history
- Sputum Culture: Identifies Haemophilus influenzae
- Blood Tests: Detects systemic inflammation (e.g., elevated white blood cells)
- Chest X-ray: Excludes pneumonia or other pulmonary abnormalities
- PCR Testing: Confirms bacterial DNA presence
Treatment of Haemophilus Influenzae Bronchitis
Treatment focuses on eradicating the bacterial infection and managing symptoms to prevent complications.
Antibiotic Therapy
Effective antibiotics against Haemophilus influenzae include:
- Beta-lactam Antibiotics: Amoxicillin-clavulanate
- Macrolides: Azithromycin, clarithromycin
- Fluoroquinolones: Levofloxacin (in severe cases)
Supportive Care
- Bronchodilators: Alleviate airway obstruction
- Hydration: Loosens mucus
- Antipyretics: Reduce fever and discomfort
Complications of Untreated Haemophilus Influenzae Bronchitis
If left untreated, Haemophilus influenzae bronchitis may progress to severe complications:
- Pneumonia
- Respiratory failure
- Chronic bronchitis
- Bacteremia
Prevention Strategies
Preventive measures reduce the risk of infection and limit bacterial transmission.
Vaccination
- Hib Vaccine: Prevents Haemophilus influenzae type b
Hygiene Practices
- Regular handwashing
- Respiratory hygiene (e.g., covering mouth while coughing)
Lifestyle Modifications
- Smoking cessation
- Managing chronic conditions
Haemophilus influenzae bronchitis is a serious bacterial respiratory infection requiring prompt diagnosis and targeted antibiotic treatment. Preventive strategies, including vaccination and lifestyle changes, are essential to reduce the incidence and complications of this condition. Individuals experiencing persistent respiratory symptoms should seek medical evaluation to ensure timely and effective management.