Haemophilus influenzae acute otitis media (AOM) is a bacterial infection affecting the middle ear, predominantly in children. It is one of the most common causes of ear infections globally and can lead to significant morbidity if untreated. This article provides a comprehensive overview of the etiology, clinical presentation, diagnostic methods, and current treatment options for Haemophilus influenzae-induced acute otitis media.
Understanding Haemophilus influenzae
Haemophilus influenzae is a facultative anaerobic, gram-negative coccobacillus. There are encapsulated (typeable) and non-encapsulated (nontypeable) strains. Nontypeable Haemophilus influenzae (NTHi) is the primary pathogen responsible for AOM, while type b (Hib) is associated with more invasive diseases such as meningitis.
Characteristics of Haemophilus influenzae:
- Gram-negative bacteria
- Facultative anaerobe (can survive with or without oxygen)
- Encapsulated and non-encapsulated strains
Pathophysiology of Haemophilus influenzae Acute Otitis Media
AOM typically arises following a viral upper respiratory tract infection (URTI). The inflammation from a URTI causes Eustachian tube dysfunction, creating an environment conducive to bacterial colonization. Nontypeable Haemophilus influenzae migrates from the nasopharynx to the middle ear, triggering an inflammatory response and fluid accumulation behind the tympanic membrane.
Clinical Presentation
Symptoms of Haemophilus influenzae AOM can develop rapidly and vary by age group. Key clinical features include:
- Otalgia (ear pain): Often the primary complaint in older children
- Otorrhea (ear discharge): Occurs if the tympanic membrane perforates
- Fever: Ranges from mild to high-grade
- Irritability and Crying: Common in infants and young children
- Hearing Loss: Temporary conductive hearing loss due to fluid buildup
Risk Factors:
- Age (6 months to 2 years)
- Attending daycare
- Exposure to tobacco smoke
- Use of pacifiers
- Family history of recurrent otitis media
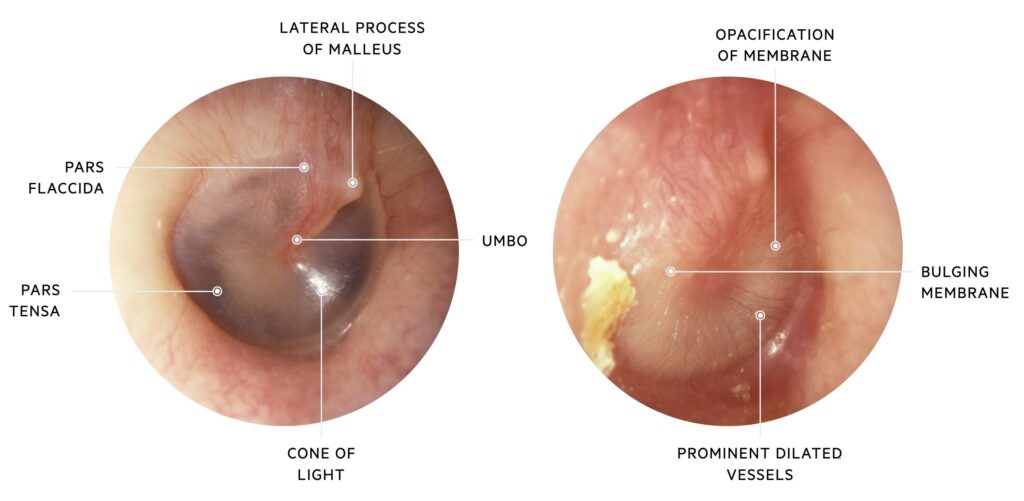
Diagnosis of Haemophilus influenzae Acute Otitis Media
Diagnosis is primarily clinical and involves a thorough history and physical examination. Diagnostic techniques include:
1. Otoscopy:
- Bulging, erythematous tympanic membrane
- Decreased or absent mobility on pneumatic otoscopy
2. Tympanocentesis (if indicated):
- Aspiration of middle ear fluid for bacterial culture
- Reserved for severe or refractory cases
3. Laboratory Testing:
- Culture and polymerase chain reaction (PCR) for definitive bacterial identification
Treatment of Haemophilus influenzae Acute Otitis Media
Timely treatment is crucial to prevent complications such as mastoiditis or hearing loss. Treatment strategies include:
1. Antibiotic Therapy:
First-line: Amoxicillin-clavulanate (covers beta-lactamase-producing H. influenzae strains)
Alternative (if allergic):
- Cefuroxime
- Cefdinir
- Azithromycin (for severe beta-lactam allergy)
2. Symptomatic Management:
- Analgesics (acetaminophen or ibuprofen) for pain relief
- Warm compresses to alleviate discomfort
3. Observation Strategy:
In select cases (mild symptoms, age >2 years), observation for 48-72 hours without antibiotics is an option.
Prevention of Haemophilus influenzae Acute Otitis Media
Preventive measures significantly reduce the incidence of Haemophilus influenzae AOM.
- Vaccination: Routine Haemophilus influenzae type b (Hib) vaccination
- Breastfeeding: Provides protective maternal antibodies
- Avoidance of Smoke Exposure: Reduces Eustachian tube dysfunction
Complications of Untreated Haemophilus influenzae Acute Otitis Media
Without proper management, H. influenzae AOM can lead to severe complications:
- Mastoiditis
- Tympanic membrane perforation
- Conductive hearing loss
- Intracranial infections (rare)
Haemophilus influenzae acute otitis media remains a prevalent pediatric infection requiring prompt diagnosis and appropriate treatment. With advancements in vaccination and antimicrobial therapies, the burden of disease can be effectively managed and reduced. Clinicians should remain vigilant for signs of complications and apply evidence-based strategies to optimize patient outcomes.
By understanding the etiology, clinical manifestations, diagnostic approaches, and treatment protocols, healthcare professionals can mitigate the impact of Haemophilus influenzae AOM and improve patient care outcomes.

