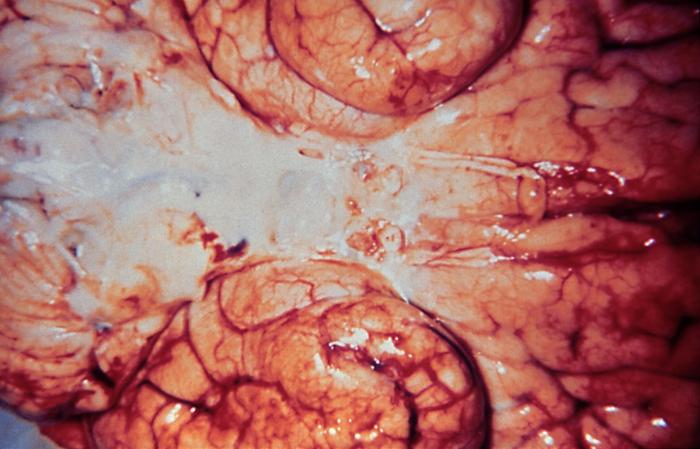
Haemophilus influenzae meningitis is a serious bacterial infection that inflames the protective membranes, or meninges, surrounding the brain and spinal cord. This condition predominantly affects infants and young children, leading to significant morbidity and mortality if not promptly addressed. Despite advancements in medical science, Haemophilus influenzae, particularly type b (Hib), remains a notable pathogen responsible for invasive diseases, including meningitis.
Etiology and Pathogenesis
Haemophilus influenzae is a Gram-negative, non-motile, coccobacillary bacterium. Among its six capsular types (a through f), type b (Hib) has been most commonly associated with severe infections. The bacterium colonizes the nasopharynx and can invade the bloodstream, crossing the blood-brain barrier to infect the meninges. Factors such as a weakened immune system or concurrent viral infections can increase susceptibility to invasive disease.
Clinical Manifestations
The onset of Haemophilus influenzae meningitis is often rapid, with symptoms including:
- Fever: Elevated body temperature.
- Headache: Severe and persistent.
- Neck Stiffness: Difficulty in bending the neck forward.
- Nausea and Vomiting: Gastrointestinal disturbances.
- Photophobia: Sensitivity to light.
- Altered Mental Status: Irritability, confusion, or lethargy.
- Seizures: Involuntary convulsions may occur in severe cases.
In infants, symptoms may be less specific, such as poor feeding, irritability, or a bulging fontanelle.
Diagnosis
Timely diagnosis is crucial for effective management. Diagnostic procedures include:
- Lumbar Puncture: Analysis of cerebrospinal fluid (CSF) to detect bacterial presence.
- Blood Cultures: Identification of bacteremia.
- Imaging Studies: CT or MRI scans to assess complications like abscess formation.
Laboratory tests focus on identifying the causative organism and determining its antibiotic susceptibility.
Treatment
Immediate initiation of empirical antibiotic therapy is essential, often before confirmatory test results are available. Recommended antibiotics include:
- Third-Generation Cephalosporins: Ceftriaxone or cefotaxime are commonly used due to their efficacy against Haemophilus influenzae.
- Beta-Lactamase Inhibitors: For strains producing beta-lactamase enzymes, combinations like ampicillin-sulbactam may be effective.
Adjunctive therapy with corticosteroids, such as dexamethasone, may reduce inflammation and the risk of neurological complications.
Prognosis and Complications
Despite appropriate treatment, Haemophilus influenzae meningitis can lead to serious complications, including:
- Neurological Sequelae: Hearing loss, cognitive impairments, or motor deficits.
- Seizure Disorders: Development of epilepsy in some cases.
- Hydrocephalus: Accumulation of CSF leading to increased intracranial pressure.
The mortality rate varies but remains significant, particularly in resource-limited settings.
Prevention
Vaccination has dramatically reduced the incidence of Hib meningitis. The Hib conjugate vaccine is recommended for infants and has proven highly effective. Additional preventive measures include:
- Immunization: Routine childhood vaccination schedules should be followed.
- Prophylactic Antibiotics: Administered to close contacts of infected individuals to prevent secondary cases.
- Infection Control Practices: Proper hygiene and respiratory etiquette to reduce transmission.
Haemophilus influenzae meningitis remains a critical public health concern. Early recognition, prompt treatment, and preventive strategies, particularly vaccination, are vital to reducing the burden of this potentially life-threatening disease.

