Gram-negative aerobic bacillary pneumonia is a severe respiratory infection primarily caused by Gram-negative bacilli. These bacteria are challenging to treat due to their robust resistance mechanisms and their ability to thrive in oxygen-rich environments. This comprehensive guide explores the causes, symptoms, risk factors, diagnosis, and treatment strategies for this serious condition.
What is Gram-Negative Aerobic Bacillary Pneumonia?
Gram-negative aerobic bacillary pneumonia refers to lung inflammation caused by Gram-negative bacteria that rely on oxygen to survive. These bacteria possess a distinctive outer membrane that makes them resistant to many antibiotics, posing a significant challenge in clinical treatment.
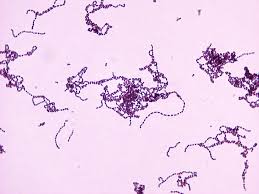
Common Gram-Negative Bacteria Involved
- Klebsiella pneumoniae
- Pseudomonas aeruginosa
- Escherichia coli (E. coli)
- Acinetobacter baumannii
- Enterobacter species
Risk Factors
Several factors elevate the risk of developing Gram-negative aerobic bacillary pneumonia, including:
- Hospitalization in Intensive Care Units (ICU)
- Mechanical ventilation
- Immunocompromised state (e.g., chemotherapy, organ transplantation)
- Chronic respiratory diseases such as COPD
- Prolonged antibiotic use
- Advanced age
Symptoms
The clinical presentation may vary, but common symptoms include:
- Persistent cough with sputum
- Chest pain during breathing or coughing
- Shortness of breath
- Fever and chills
- Fatigue and weakness
- Confusion (especially in elderly patients)
Diagnosis
Accurate diagnosis requires a combination of clinical evaluation, imaging studies, and microbiological testing.
Diagnostic Methods
- Chest X-ray: Identifies lung consolidation or infiltrates
- CT Scan: Provides detailed imaging for severe cases
- Blood Tests: Detect elevated white blood cell counts
- Sputum Culture: Identifies the causative bacterial strain
- Bronchoscopy: Used for sample collection in severe or non-responsive cases
Treatment Strategies
Effective treatment for Gram-negative aerobic bacillary pneumonia requires targeted antibiotic therapy, supportive care, and infection control measures.
Antibiotic Therapy
Given the resistance profile of Gram-negative bacteria, treatment often includes:
- Carbapenems (e.g., meropenem, imipenem)
- Piperacillin-tazobactam
- Cefepime
- Colistin (for multi-drug resistant strains)
- Combination therapies to enhance efficacy and reduce resistance risks
Supportive Care
- Oxygen therapy to maintain blood oxygen levels
- Mechanical ventilation in severe respiratory failure cases
- Fluid management to maintain hydration and stabilize blood pressure
Infection Control Measures
- Hand hygiene protocols
- Isolation practices for patients with multi-drug resistant infections
- Environmental disinfection in healthcare settings
Complications
If untreated, Gram-negative aerobic bacillary pneumonia may lead to:
- Sepsis
- Lung abscesses
- Respiratory failure
- Pleural effusion (fluid buildup in the chest cavity)
Prevention
Preventive strategies are crucial in reducing the incidence of Gram-negative aerobic bacillary pneumonia.
Key Preventive Measures
- Vaccination for influenza and pneumococcus
- Proper hand hygiene to prevent bacterial transmission
- Early weaning from ventilators to reduce ventilator-associated pneumonia risk
- Antibiotic stewardship programs to minimize resistance development
Prognosis
The prognosis depends on early diagnosis, appropriate treatment, and the patient’s overall health. Patients with weakened immune systems or pre-existing conditions may face a higher risk of complications.
FAQs
What are the most common causes of Gram-negative aerobic bacillary pneumonia?
Klebsiella pneumoniae, Pseudomonas aeruginosa, and Escherichia coli are the leading causes.
Is Gram-negative pneumonia contagious?
While not typically contagious through casual contact, healthcare-associated infections can spread in hospitals if infection control protocols are inadequate.
What is the mortality rate for Gram-negative aerobic bacillary pneumonia?
The mortality rate varies depending on comorbidities, bacterial resistance, and treatment speed. Severe cases, especially in ICUs, can have mortality rates exceeding 30%.
How is this condition different from viral pneumonia?
Gram-negative aerobic bacillary pneumonia is bacterial in origin, whereas viral pneumonia results from viruses like influenza or SARS-CoV-2. Antibiotic treatment is crucial for bacterial pneumonia.
Can Gram-negative pneumonia be prevented in high-risk patients?
Yes, preventive measures such as infection control protocols, vaccination, and antibiotic stewardship significantly reduce the risk in vulnerable patients.