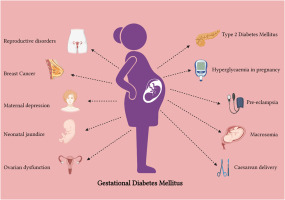
Gestational diabetes mellitus (GDM) is a form of diabetes diagnosed during pregnancy that was not present before conception. It affects how the body processes glucose, often resulting in high blood sugar levels. While GDM usually resolves after childbirth, it requires careful management to ensure the health of both mother and baby.
Causes of Gestational Diabetes Mellitus
GDM develops when hormonal changes during pregnancy cause insulin resistance. The placenta produces hormones such as human placental lactogen (hPL) and cortisol, which impair insulin function. As a result, the body struggles to effectively use glucose, leading to elevated blood sugar levels.
Risk Factors
- Obesity or overweight
- Family history of diabetes
- Age over 25
- Polycystic ovary syndrome (PCOS)
- Previous GDM diagnosis
- Ethnic background (e.g., African, Asian, Hispanic)
Symptoms of Gestational Diabetes Mellitus
While GDM may not present noticeable symptoms, some women may experience:
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
- Frequent infections
Diagnosis of Gestational Diabetes Mellitus
Screening Tests
- Glucose Challenge Test (GCT): A non-fasting test where a glucose solution is consumed, followed by a blood sugar measurement after one hour.
- Oral Glucose Tolerance Test (OGTT): A fasting test that involves consuming a glucose solution and measuring blood sugar levels at intervals.
Complications of Gestational Diabetes Mellitus
Untreated GDM can result in several complications:
- For the Baby:
- Macrosomia (excessive birth weight)
- Hypoglycemia (low blood sugar)
- Premature birth
- Respiratory distress syndrome
- For the Mother:
- Preeclampsia
- Increased risk of type 2 diabetes
Management and Treatment
Lifestyle Modifications
- Healthy Diet: A balanced diet rich in fiber, lean protein, and complex carbohydrates can help stabilize blood sugar.
- Regular Exercise: Engaging in moderate physical activities like walking or swimming aids glucose metabolism.
Medical Treatment
- Blood Sugar Monitoring: Frequent testing helps maintain optimal glucose levels.
- Insulin Therapy: If lifestyle changes are insufficient, insulin may be required to control blood sugar.
- Oral Medications: Metformin or glyburide may be prescribed in certain cases.
Dietary Recommendations
- Focus on low-glycemic index foods
- Incorporate whole grains, vegetables, and fruits
- Avoid processed sugars and refined carbohydrates
Postpartum Care and Follow-up
Women diagnosed with GDM should undergo a glucose tolerance test 6-12 weeks postpartum to assess long-term diabetes risk. Lifelong monitoring and adopting a healthy lifestyle reduce the risk of developing type 2 diabetes.
Preventive Measures
- Maintain a healthy weight before pregnancy
- Engage in regular exercise
- Follow a balanced diet
- Monitor blood sugar levels during pregnancy if at high risk
FAQs:
Can gestational diabetes be prevented?
While it cannot always be prevented, maintaining a healthy lifestyle before and during pregnancy significantly reduces the risk.
Is gestational diabetes harmful to the baby?
If managed well, the risks to the baby are minimal. However, untreated GDM can lead to complications like excessive birth weight and respiratory issues.
Does gestational diabetes mean I will develop type 2 diabetes?
Women with GDM have a higher risk of developing type 2 diabetes later in life. Regular screening and healthy habits can mitigate this risk.
What foods should I avoid with gestational diabetes?
Avoid sugary snacks, refined carbohydrates, and heavily processed foods. Focus on whole grains, lean proteins, and fiber-rich vegetables.
How often should I check my blood sugar with GDM?
Your doctor will advise a suitable schedule, typically involving fasting, post-meal, and bedtime glucose checks.