Acute adrenocortical insufficiency, also known as adrenal crisis, is a life-threatening condition that occurs due to an acute deficiency of cortisol and other essential adrenal hormones. It requires immediate medical intervention to prevent severe complications. This guide provides an in-depth overview of the condition, covering its causes, symptoms, diagnostic approaches, and treatment strategies.
Understanding Acute Adrenocortical Insufficiency
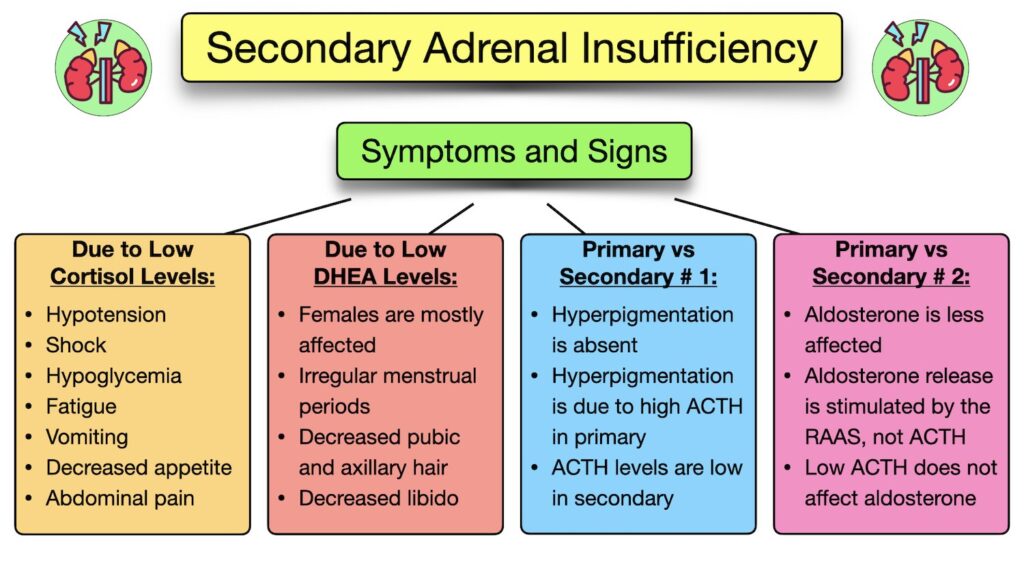
Acute adrenocortical insufficiency occurs when the adrenal glands fail to produce adequate amounts of cortisol, a hormone critical for managing stress, maintaining blood pressure, and regulating metabolism. This insufficiency can arise abruptly in individuals with adrenal gland disorders or during periods of stress in those with underlying adrenal insufficiency.
Causes of Acute Adrenocortical Insufficiency
The condition may result from several factors:
- Adrenal Gland Damage: Destruction of adrenal tissue due to autoimmune diseases (e.g., Addison’s disease), infections, or hemorrhage.
- Sudden Discontinuation of Corticosteroids: Abruptly stopping long-term corticosteroid therapy can suppress the hypothalamic-pituitary-adrenal (HPA) axis, leading to acute insufficiency.
- Infections and Illnesses: Severe infections like sepsis or meningitis can impair adrenal function or increase cortisol demand, leading to a crisis.
- Surgical Procedures or Trauma: Stressful events such as surgery or injury in patients with undiagnosed or untreated adrenal insufficiency can trigger an adrenal crisis.
Key Symptoms of Adrenal Crisis
Symptoms of acute adrenocortical insufficiency develop rapidly and can include:
- Severe fatigue and weakness
- Hypotension (low blood pressure) unresponsive to fluids
- Hypoglycemia (low blood sugar)
- Nausea, vomiting, and abdominal pain
- Confusion, dizziness, or loss of consciousness
- Electrolyte imbalances, such as hyponatremia (low sodium) and hyperkalemia (high potassium)
Diagnostic Approaches for Acute Adrenocortical Insufficiency
Timely diagnosis of adrenal crisis is critical. Diagnostic evaluations include:
1. Clinical Assessment
Healthcare providers assess the patient’s history, symptoms, and physical examination findings to identify signs consistent with adrenal insufficiency.
2. Laboratory Tests
- Cortisol Levels: Serum cortisol levels are measured to confirm cortisol deficiency.
- ACTH Levels: High levels of adrenocorticotropic hormone (ACTH) suggest primary adrenal insufficiency, while low levels may indicate secondary insufficiency.
- Electrolyte Panel: Imbalances, including hyponatremia and hyperkalemia, are common indicators of adrenal dysfunction.
3. ACTH Stimulation Test
The ACTH stimulation test assesses adrenal gland responsiveness by measuring cortisol levels before and after administration of synthetic ACTH. A blunted response confirms adrenal insufficiency.
Treatment and Management of Adrenal Crisis
Prompt treatment is essential to avoid life-threatening complications. Management strategies include:
1. Immediate Hormonal Replacement
- Hydrocortisone: Intravenous hydrocortisone is the first-line treatment to replenish cortisol levels and manage symptoms. It is typically administered in high doses initially, followed by tapering as the crisis resolves.
- Fludrocortisone: For patients with primary adrenal insufficiency, fludrocortisone may be added to replace mineralocorticoid deficiency.
2. Fluid and Electrolyte Management
Intravenous saline and glucose solutions are used to correct dehydration, hypotension, and hypoglycemia. Electrolyte imbalances, such as hyperkalemia, are managed with appropriate interventions.
3. Infection Control
If the crisis is triggered by infection, prompt treatment with antibiotics or antiviral medications is necessary to control the underlying cause.
4. Monitoring and Support
Continuous monitoring of vital signs, glucose levels, and electrolytes is critical to ensure stabilization during recovery.
Prevention of Acute Adrenocortical Insufficiency
Preventive measures are vital for at-risk individuals:
1. Patient Education
Patients with adrenal insufficiency should be educated about recognizing early symptoms of adrenal crisis and the importance of carrying medical identification (e.g., a bracelet).
2. Steroid Replacement Therapy
Patients on long-term corticosteroids should receive appropriate maintenance doses and guidance on dose adjustments during stress, illness, or surgery.
3. Emergency Preparedness
At-risk patients should carry an emergency injection kit with hydrocortisone and know how to use it during a crisis. Family members and caregivers should also be trained to administer the injection.
4. Regular Monitoring
Routine follow-ups with healthcare providers ensure proper management of adrenal insufficiency and timely adjustments to therapy.
Acute adrenocortical insufficiency is a medical emergency that requires rapid identification and intervention. Healthcare providers play a critical role in managing this condition through timely treatment, patient education, and preventive measures. By understanding the causes, symptoms, and treatment options, we can improve outcomes and ensure patients receive optimal care during an adrenal crisis.