Gastrointestinal anthrax is a rare but serious manifestation of infection by Bacillus anthracis, a spore-forming bacterium. This form of anthrax occurs following the ingestion of contaminated meat and can affect any part of the gastrointestinal tract, leading to severe clinical outcomes. Understanding its etiology, clinical presentation, diagnostic approaches, treatment options, and preventive measures is crucial for effective management and control.

Etiology and Pathogenesis
Bacillus anthracis spores are highly resilient and can survive in harsh environmental conditions for extended periods. Gastrointestinal anthrax typically results from consuming undercooked or raw meat from infected animals. Once ingested, the spores can germinate in the gastrointestinal tract, releasing toxins that cause local ulcerations, edema, and systemic manifestations.
Clinical Manifestations
The clinical presentation of gastrointestinal anthrax varies depending on the site of infection within the gastrointestinal tract:
- Oropharyngeal Anthrax: Infection in the oral cavity, particularly the tonsils and posterior pharynx, leads to sore throat, dysphagia, and significant neck swelling due to lymphadenopathy and edema.
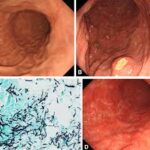
- Intestinal Anthrax: Involvement of the stomach and intestines presents with nonspecific symptoms such as nausea, vomiting, anorexia, and fever. As the disease progresses, patients may experience severe abdominal pain, hematemesis, bloody diarrhea, and signs of acute abdomen due to complications like hemorrhage, perforation, or obstruction.
Diagnostic Approaches
Diagnosing gastrointestinal anthrax is challenging due to its nonspecific initial symptoms. A high index of suspicion is essential, especially in endemic areas or following consumption of potentially contaminated meat. Diagnostic methods include:
- Microbiological Cultures: Isolation of B. anthracis from blood, stool, or affected tissues confirms the diagnosis.
- Imaging Studies: Abdominal imaging may reveal bowel wall thickening, ascites, or lymphadenopathy, aiding in assessing disease extent and complications.
Treatment Strategies
Early initiation of antibiotic therapy is critical for improving outcomes:
- Antibiotics: Empirical treatment often includes a combination of ciprofloxacin or doxycycline with one or two additional agents such as penicillin, vancomycin, or rifampin.
- Supportive Care: Management of shock, fluid and electrolyte imbalances, and organ dysfunction is vital.
- Surgical Intervention: Indicated for patients with complications like bowel perforation or significant hemorrhage.
Prevention and Control
Preventive measures focus on reducing exposure to B. anthracis spores:
- Food Safety: Ensuring proper cooking of meat, especially in regions where anthrax is endemic, to inactivate spores.
- Public Health Surveillance: Monitoring and controlling anthrax in livestock populations to prevent transmission to humans.
- Education: Raising awareness among communities about the risks associated with handling and consuming meat from potentially infected animals.
Gastrointestinal anthrax, though rare, poses significant health risks due to its severe clinical manifestations and high mortality rate if not promptly treated. Early recognition, timely antibiotic therapy, supportive care, and preventive strategies are essential components in managing and controlling this life-threatening infection.