Gastroenteritis due to Shigella, commonly referred to as shigellosis, represents a significant public health concern worldwide. This bacterial infection primarily affects the intestines, leading to severe gastrointestinal distress. Understanding its etiology, clinical manifestations, diagnostic approaches, treatment options, and preventive measures is crucial for effective management and control.
Etiology of Shigella-Induced Gastroenteritis
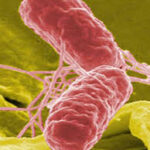
Shigella is a genus of Gram-negative, non-motile, facultatively anaerobic bacteria responsible for shigellosis. The four primary species affecting humans are:
- Shigella dysenteriae: Noted for causing severe epidemics, this species produces Shiga toxin, leading to severe dysentery and potential complications such as hemolytic uremic syndrome.
- Shigella flexneri: Predominant in developing countries, it often results in endemic infections.
- Shigella boydii: Less common but still a notable pathogen in certain regions.
- Shigella sonnei: More prevalent in industrialized nations, accounting for a significant portion of shigellosis cases.
Transmission occurs via the fecal-oral route, often through consumption of contaminated food or water, or direct person-to-person contact. A remarkably low infectious dose is required to cause illness; ingestion of fewer than 100 bacterial cells can lead to infection.
Clinical Manifestations
Symptoms typically manifest one to two days post-exposure and may include:
- Diarrhea: Often bloody, indicative of colonic involvement.
- Abdominal pain and cramps: Resulting from intestinal inflammation.
- Fever: Reflecting the body’s immune response to infection.
- Tenesmus: A distressing sensation of incomplete bowel evacuation.
In some cases, especially among young children and the elderly, complications such as dehydration, seizures, and reactive arthritis may arise.
Diagnostic Approaches
Accurate diagnosis is paramount for effective treatment and involves:
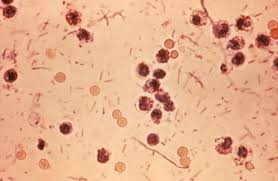
- Stool Culture: Isolation and identification of Shigella species from fecal samples remain the gold standard.
- Molecular Techniques: Polymerase Chain Reaction (PCR) assays enhance detection sensitivity and specificity.
- Antimicrobial Susceptibility Testing: Essential due to increasing antibiotic resistance among Shigella strains.
Treatment Modalities
Management strategies focus on:
- Rehydration: Oral rehydration solutions are vital to counteract dehydration resulting from diarrhea.
- Antibiotic Therapy: Indicated in severe cases or for specific populations (e.g., immunocompromised individuals). Common antibiotics include ciprofloxacin and azithromycin; however, resistance patterns necessitate susceptibility testing prior to administration.
- Symptomatic Relief: Antipyretics and antispasmodics may be employed to alleviate discomfort.
Preventive Measures
Preventing shigellosis hinges on:
- Proper Hygiene Practices: Regular and thorough handwashing with soap and water, especially after using the restroom and before handling food.
- Safe Food Handling: Ensuring food is prepared and stored under sanitary conditions to prevent contamination.
- Access to Clean Water: Utilizing treated water sources for drinking and cooking purposes.
- Public Health Education: Raising awareness about transmission routes and preventive strategies.
Pathogenesis of Shigella Infection
The pathogenicity of Shigella involves several key mechanisms:
- Invasion of Colonic Epithelium: Shigella species invade the epithelial lining of the colon, leading to cell death and inflammation.
- Toxin Production: Certain strains produce toxins, such as the Shiga toxin by S. dysenteriae, contributing to disease severity.
- Intracellular Replication: After invasion, Shigella multiplies within host cells and spreads to adjacent cells, causing extensive tissue damage.
Gastroenteritis due to Shigella remains a pressing global health issue. Comprehensive understanding of its transmission, clinical presentation, diagnostic methods, treatment options, and preventive measures is essential for healthcare professionals and the public alike. Emphasizing hygiene, safe food practices, and prompt medical attention can significantly reduce the burden of this infection.