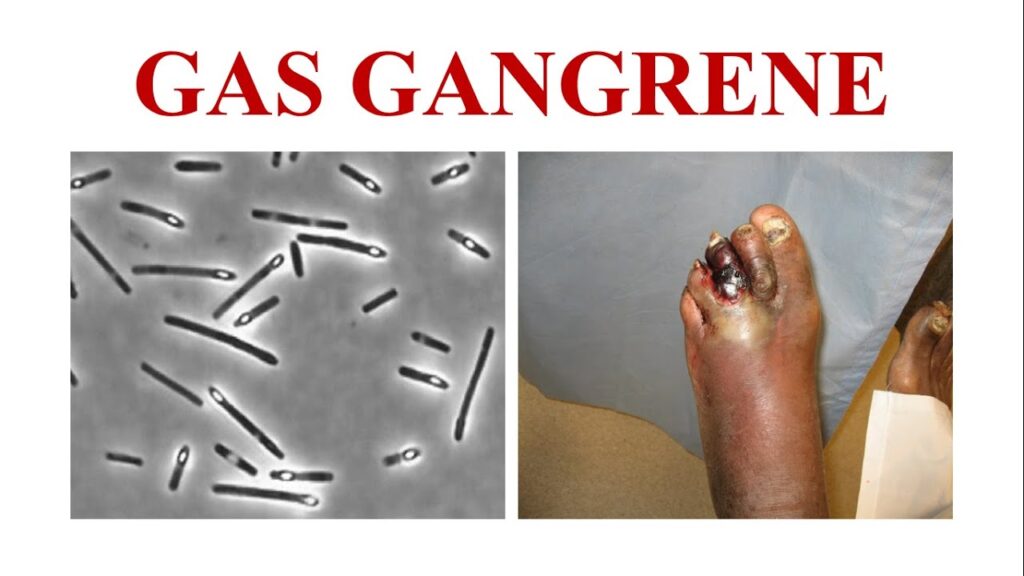
Gas gangrene, also known as clostridial myonecrosis, is a severe and potentially fatal bacterial infection primarily caused by Clostridium perfringens. This anaerobic, spore-forming bacterium rapidly multiplies in devitalized tissue, producing toxins that cause extensive tissue necrosis, gas formation, and systemic toxicity. Immediate medical intervention is critical to prevent mortality.
Causes and Pathogenesis of Gas Gangrene
Gas gangrene occurs when C. perfringens infects deep wounds with low oxygen levels, creating an ideal anaerobic environment for bacterial proliferation. The bacteria produce potent exotoxins, such as alpha toxin (phospholipase C) and theta toxin, which:
- Destroy cell membranes, leading to widespread necrosis
- Increase vascular permeability, causing edema and impaired blood flow
- Induce hemolysis, leading to systemic toxicity and multi-organ failure
Common Risk Factors
- Traumatic injuries: Deep penetrating wounds, gunshot wounds, or crush injuries
- Surgical procedures: Contaminated surgeries, bowel surgeries, or C-sections
- Diabetes and vascular diseases: Poor circulation promotes anaerobic bacterial growth
- Immunosuppression: Chemotherapy, HIV, or chronic diseases increase susceptibility
Clinical Manifestations of Gas Gangrene
The onset of symptoms is rapid, often within 6 to 48 hours after infection. Common signs include:
Early Symptoms
- Severe pain at the infection site, disproportionate to the wound appearance
- Swelling and erythema, progressing to skin discoloration
- Crepitus (gas under the skin), caused by bacterial gas production
Advanced Symptoms
- Foul-smelling discharge, often serosanguinous
- Bullae formation, with hemorrhagic fluid
- Systemic toxicity, including fever, tachycardia, hypotension, and altered mental status
- Shock and multi-organ failure, if untreated
Diagnosis of Gas Gangrene
Early and accurate diagnosis is crucial for survival. Diagnostic methods include:
Clinical Assessment
- Rapidly progressing soft tissue necrosis with crepitus
- Presence of a foul odor and purulent discharge
Imaging Studies
- X-ray and CT scan: Reveal gas bubbles in soft tissue
- MRI: Helps differentiate necrotizing infections from other soft tissue infections
Microbiological Tests
- Gram stain: Identifies gram-positive bacilli without inflammatory response
- Anaerobic cultures: Confirm C. perfringens presence, though cultures may take time
- Toxin assays: Detect lethal C. perfringens exotoxins in blood or tissue
Treatment and Management of Gas Gangrene
Immediate Surgical Debridement
- Wide excision of necrotic tissue is mandatory
- Amputation may be required in severe cases to prevent systemic spread
Antibiotic Therapy
- High-dose intravenous penicillin G (first-line treatment)
- Clindamycin (inhibits toxin production) as an adjunct therapy
- Metronidazole or carbapenems for polymicrobial infections
Hyperbaric Oxygen Therapy (HBOT)
- Increases tissue oxygenation, inhibiting anaerobic bacterial growth
- Enhances antibiotic efficacy and immune response
Supportive Care
- Intravenous fluids and vasopressors for hemodynamic support
- Pain management and wound care
- Blood transfusions in cases of severe hemolysis
Complications and Prognosis
If untreated, gas gangrene has a mortality rate exceeding 50%. Even with aggressive treatment, complications may include:
- Septic shock and multi-organ failure
- Permanent limb loss due to extensive debridement
- Recurrent infections requiring prolonged medical care
Timely intervention significantly improves survival rates, with early recognition and aggressive management reducing fatality risks.
Prevention Strategies
- Proper wound care: Immediate cleaning and debridement of contaminated wounds
- Prophylactic antibiotics: For high-risk surgeries and deep injuries
- Diabetes and vascular disease management: Reducing susceptibility to infections
- Early medical attention: Promptly addressing signs of infection before progression
Gas gangrene caused by Clostridium perfringens is a rapidly progressing, life-threatening infection requiring immediate medical intervention. Early recognition, aggressive surgical debridement, targeted antibiotic therapy, and hyperbaric oxygen therapy significantly improve patient outcomes. Awareness and preventive measures are crucial in reducing the incidence of this severe bacterial infection.