Acutely decompensated chronic heart failure (ADCHF) is a critical condition characterized by the sudden worsening of heart failure symptoms. It requires immediate medical attention to prevent life-threatening complications.
Pathophysiology of Acutely Decompensated Chronic Heart Failure
ADCHF occurs due to a rapid decline in the heart’s ability to pump blood efficiently, leading to congestion and inadequate perfusion of vital organs. Various triggers can exacerbate pre-existing chronic heart failure, causing acute deterioration.
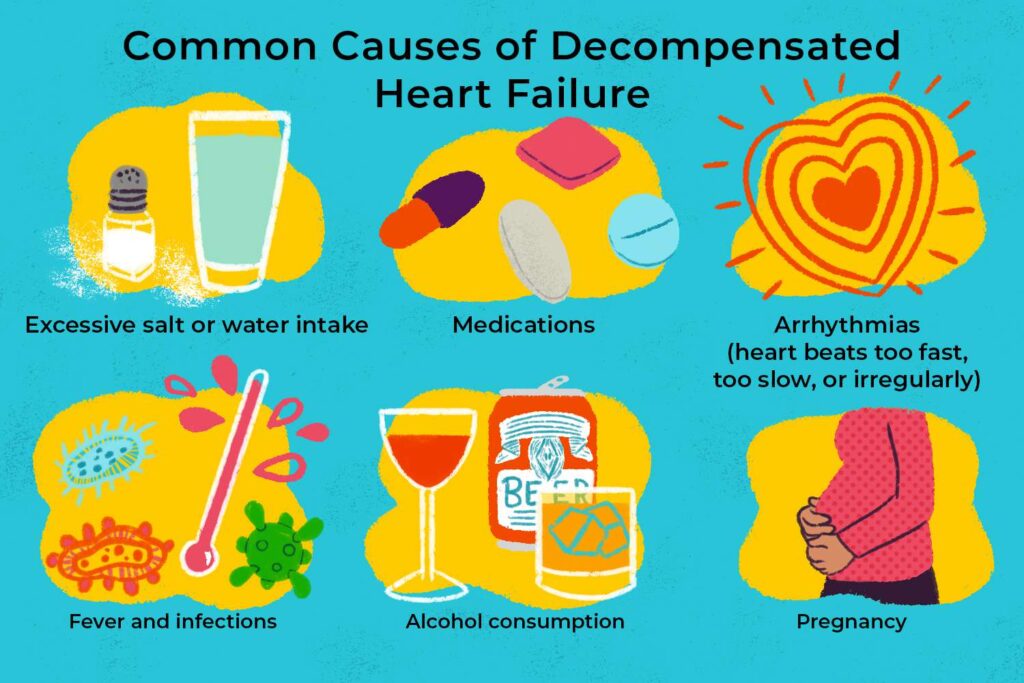
Causes and Risk Factors
1. Cardiac Causes
- Myocardial infarction
- Arrhythmias (e.g., atrial fibrillation)
- Uncontrolled hypertension
2. Non-Cardiac Causes
- Pulmonary infections
- Renal dysfunction
- Anemia
3. Lifestyle and Medication Factors
- Non-adherence to medication
- Excessive sodium or fluid intake
- Alcohol and drug use
Symptoms of Acutely Decompensated Chronic Heart Failure
- Severe Dyspnea: Shortness of breath, especially at rest
- Pulmonary Edema: Fluid accumulation in the lungs
- Peripheral Edema: Swelling in the legs and feet
- Fatigue and Weakness: Reduced oxygen delivery to tissues
- Hypotension or Hypertension: Depending on the underlying cause
- Altered Mental Status: In severe cases due to reduced cerebral perfusion
Diagnostic Approach
1. Clinical Assessment
- Comprehensive history and physical examination
- New York Heart Association (NYHA) classification
2. Imaging Studies
- Chest X-ray: Identifies pulmonary congestion and cardiomegaly
- Echocardiography: Assesses ejection fraction and valvular function
- Electrocardiogram (ECG): Detects arrhythmias or ischemic changes
3. Laboratory Tests
- B-type Natriuretic Peptide (BNP) or NT-proBNP levels
- Arterial blood gas (ABG) analysis
- Serum electrolytes, renal function, and liver enzymes
Treatment Strategies
1. Acute Management
- Oxygen Therapy: For hypoxia
- Diuretics (e.g., Furosemide): To reduce fluid overload
- Vasodilators (e.g., Nitroglycerin): To decrease preload and afterload
- Inotropes (e.g., Dobutamine): In cases of cardiogenic shock
2. Long-Term Management
- Beta-Blockers: To improve cardiac function
- ACE Inhibitors or ARBs: To reduce afterload and prevent remodeling
- Aldosterone Antagonists: For fluid balance control
3. Lifestyle and Preventive Strategies
- Dietary Modifications: Sodium restriction and fluid management
- Regular Exercise: As tolerated by the patient
- Medication Adherence: Ensuring compliance with prescribed treatments
Prognosis and Complications
Favorable Prognostic Factors
- Early intervention and hospital management
- Stable cardiac function post-discharge
- Effective long-term treatment adherence
Adverse Prognostic Factors
- Recurrent hospitalizations
- Persistent fluid overload
- Comorbid conditions (e.g., renal failure, diabetes)
Potential Complications
- Pulmonary edema
- Cardiogenic shock
- Multi-organ failure
Acutely decompensated chronic heart failure is a medical emergency requiring immediate treatment. Early recognition, aggressive management, and long-term care strategies significantly improve patient outcomes and reduce hospital readmissions.

