Eumycotic mycetoma is a chronic, progressively destructive fungal infection affecting the skin, subcutaneous tissues, and bones. It primarily occurs in tropical and subtropical regions and is commonly seen in agricultural workers due to soil-borne fungal exposure. Unlike actinomycotic mycetoma, which is caused by bacteria, eumycotic mycetoma is caused by various fungi, leading to severe morbidity if left untreated.
Causes and Pathogens
Eumycotic mycetoma is caused by several fungal species, including:
- Madurella mycetomatis
- Madurella grisea
- Falciformispora senegalensis
- Trematosphaeria grisea
- Aspergillus spp.
These fungi are found in soil and enter the body through minor trauma, often on the feet or hands.
Pathophysiology
Upon inoculation, fungi form colonies and trigger an immune response, leading to chronic inflammation and the development of granulomatous lesions. The infection spreads through contiguous tissue planes, causing:
- Fibrosis
- Sinus tract formation
- Bone destruction (osteolysis)
- Formation of characteristic fungal grains in tissue
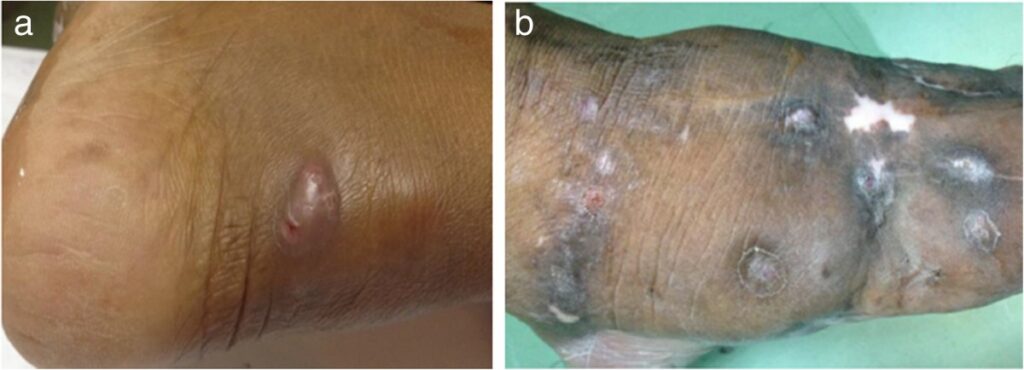
Clinical Manifestations
Early Symptoms:
- Painless swelling at the infection site
- Formation of nodules and subcutaneous abscesses
- Skin discoloration (erythema or hyperpigmentation)
Advanced Symptoms:
- Multiple draining sinuses discharging granules (black, white, or yellow fungal grains)
- Ulceration and secondary bacterial infection
- Deformity and restricted mobility due to fibrotic tissue changes
Diagnosis
Timely diagnosis is crucial to prevent severe complications. The following methods aid in confirming eumycotic mycetoma:
1. Clinical Examination:
- Observation of classical triad: swelling, sinuses, and granules
- History of trauma or barefoot walking in endemic regions
2. Laboratory Investigations:
- Direct Microscopy: KOH mount to detect fungal elements in grains
- Histopathology: PAS/GMS staining for fungal hyphae
- Culture: Growth on Sabouraud’s dextrose agar
- Molecular Testing: PCR-based fungal identification
3. Imaging Studies:
- X-ray: Detects bone involvement
- Ultrasound: Identifies lesions and fluid collections
- MRI/CT Scan: Provides detailed soft tissue and bone involvement assessment
Treatment Options
1. Antifungal Therapy
- First-line antifungals:
- Itraconazole (200-400 mg/day)
- Voriconazole (used in refractory cases)
- Amphotericin B for severe infections
- Long-term therapy required (6-12 months or more)
2. Surgical Intervention
- Debridement of necrotic tissue
- Limb amputation in extreme cases with irreversible damage
3. Adjunctive Therapy
- Wound care and antibiotics for secondary infections
- Physiotherapy to restore mobility post-surgery
Prevention and Control
- Wearing protective footwear in endemic areas
- Immediate treatment of minor skin injuries
- Public health education on early symptom recognition