What Is Essential Thrombocythemia?
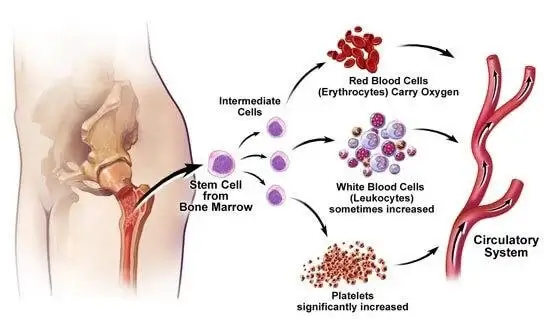
Essential thrombocythemia (ET) is a rare chronic blood disorder characterized by an abnormally high number of platelets in the blood. It is classified as a myeloproliferative neoplasm (MPN), meaning it results from the overproduction of blood cells in the bone marrow. ET increases the risk of blood clots (thrombosis) and, in some cases, bleeding complications.
Causes and Risk Factors
While the exact cause of ET remains unclear, genetic mutations play a significant role. The most common mutations associated with ET include:
- JAK2 Mutation: Present in approximately 50-60% of ET cases, this mutation causes abnormal signaling pathways, leading to excessive platelet production.
- CALR Mutation: Found in about 20-30% of cases, this mutation affects the calreticulin protein, influencing blood cell production.
- MPL Mutation: Detected in 5-10% of cases, this mutation impacts the thrombopoietin receptor, which regulates platelet production.
Other risk factors include:
- Age (most common in individuals over 50 but can occur in younger adults)
- Gender (more frequent in women)
- Family history of MPNs
Symptoms of Essential Thrombocythemia
ET may be asymptomatic in many individuals, but when symptoms occur, they typically include:
- Thrombosis (Blood Clots): Increased platelet count raises the risk of clot formation, leading to complications like strokes, heart attacks, or deep vein thrombosis (DVT).
- Microvascular Symptoms: Tingling, burning sensations in hands and feet (erythromelalgia), headaches, dizziness, or visual disturbances.
- Bleeding Issues: Paradoxically, excessive platelets can lead to bleeding problems such as nosebleeds, gum bleeding, or bruising.
- Splenomegaly (Enlarged Spleen): Some individuals may experience abdominal discomfort due to spleen enlargement.
Diagnosis and Medical Evaluation
ET is typically diagnosed through blood tests and bone marrow analysis. The diagnostic process includes:
Blood Tests:
- Complete Blood Count (CBC): Elevated platelet count (above 450,000 per microliter of blood)
- Genetic Testing: Detection of JAK2, CALR, or MPL mutations
- Peripheral Blood Smear: Examines the appearance of platelets and other blood cells
Bone Marrow Biopsy:
A biopsy may be performed to confirm ET by analyzing bone marrow cellularity, megakaryocyte proliferation, and fibrosis levels.
Differential Diagnosis:
ET must be distinguished from other conditions causing thrombocytosis, including:
- Reactive (secondary) thrombocytosis (due to infections, inflammation, iron deficiency, or cancer)
- Other MPNs like polycythemia vera (PV) or primary myelofibrosis (PMF)
Treatment Options for Essential Thrombocythemia
Treatment depends on an individual’s risk of complications and symptoms.
Low-Risk Patients (Younger than 60, No History of Blood Clots, JAK2-Negative)
- Aspirin Therapy: Low-dose aspirin reduces clotting risk by preventing platelet aggregation.
- Monitoring: Regular blood tests to track platelet levels.
High-Risk Patients (Over 60, History of Thrombosis, JAK2-Positive)
- Cytoreductive Therapy: Medications to lower platelet counts, including:
- Hydroxyurea: First-line treatment for high-risk patients
- Anagrelide: Alternative for patients intolerant to hydroxyurea
- Interferon-alpha: Preferred in younger patients and pregnant women
- Antiplatelet Therapy: Aspirin combined with cytoreductive drugs
Experimental and Advanced Therapies
- JAK2 Inhibitors: Ruxolitinib and other targeted therapies are under investigation for ET treatment.
- Stem Cell Transplantation: Rarely used, considered for cases progressing to myelofibrosis or leukemia.
Complications and Prognosis
While ET is generally manageable, complications can arise, including:
- Thrombotic Events: Stroke, myocardial infarction, pulmonary embolism
- Hemorrhagic Complications: Uncontrolled bleeding despite high platelet count
- Progression to Myelofibrosis or Leukemia: Rare but possible in long-term cases
Prognosis
Most individuals with ET have a normal life expectancy with proper management. The risk of severe complications can be minimized with regular monitoring and appropriate treatment.
Lifestyle and Management Strategies
While medical treatment is essential, lifestyle adjustments can further help manage ET:
- Healthy Diet: Anti-inflammatory foods, adequate hydration, and balanced nutrition
- Regular Exercise: Improves circulation and reduces clot risk
- Smoking Cessation: Smoking increases thrombosis risk
- Routine Medical Checkups: Ensures timely intervention for emerging complications

