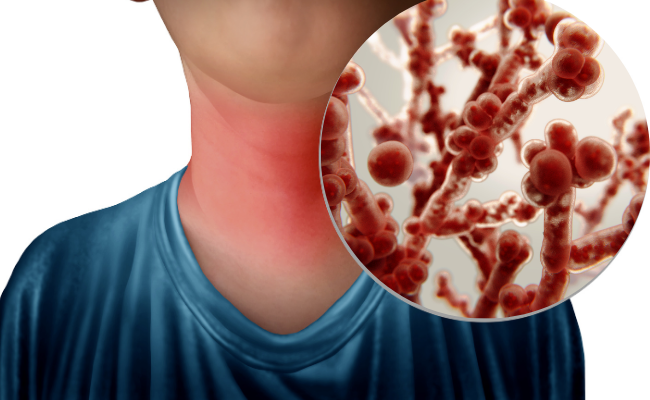
Esophageal candidiasis, also known as Candida esophagitis, is a fungal infection caused by Candida species, primarily Candida albicans. It commonly affects immunocompromised individuals, such as those with HIV/AIDS, cancer, or diabetes, and patients on immunosuppressive therapy. This condition can lead to significant discomfort and complications if left untreated.
Causes and Risk Factors
Candida species are normal commensals of the gastrointestinal tract, but under certain conditions, they proliferate and cause infection. The primary risk factors include:
- Weakened Immune System: HIV/AIDS, chemotherapy, organ transplantation
- Uncontrolled Diabetes Mellitus: High blood sugar levels promote fungal overgrowth
- Corticosteroid and Immunosuppressive Therapy: Asthma inhalers, post-transplant medications
- Prolonged Antibiotic Use: Disrupts normal bacterial flora, allowing fungal overgrowth
- Gastroesophageal Reflux Disease (GERD): Damage to the esophageal mucosa facilitates infection
- Malnutrition: Deficiency in essential nutrients weakens immune defenses
Symptoms of Esophageal Candidiasis
Common clinical manifestations include:
- Odynophagia (Painful Swallowing): Sharp pain during swallowing, particularly with solid foods
- Dysphagia (Difficulty Swallowing): Sensation of food sticking in the esophagus
- Retro-sternal Pain: Burning discomfort behind the breastbone
- Oral Thrush: White patches in the mouth, often coexisting with esophageal infection
- Weight Loss and Malnutrition: Resulting from difficulty eating and decreased food intake
Diagnosis
Diagnosis is based on clinical symptoms, endoscopic findings, and laboratory tests:
- Endoscopy with Biopsy: White plaque-like lesions on the esophageal mucosa; biopsy confirms fungal invasion.
- Cytology and Culture: Microscopic examination and fungal culture from biopsy samples.
- Barium Swallow Study: Identifies structural abnormalities but is less specific than endoscopy.
- Serological Tests: Used in systemic fungal infections but not routinely required.
Treatment Options
First-Line Therapy
- Fluconazole (Oral or IV): 100-400 mg/day for 14-21 days
- Itraconazole Oral Solution: Alternative for fluconazole-resistant cases
Refractory or Severe Cases
- Voriconazole or Posaconazole: Used in fluconazole-resistant Candida infections
- Amphotericin B (IV): Reserved for severe, systemic cases
Adjunctive Measures
- Nystatin Oral Suspension: Helps control concurrent oral thrush
- Dietary Modifications: Soft, non-irritating foods to ease swallowing
Prevention Strategies
- Good Oral Hygiene: Regular brushing and antifungal mouth rinses for at-risk individuals
- Proper Use of Inhaled Steroids: Rinse mouth after use to prevent fungal overgrowth
- Blood Sugar Control: Essential for diabetics to prevent recurrent infections
- Probiotic Use: Helps maintain gut flora balance and reduce Candida colonization