B-cell acute lymphoblastic leukemia (B-ALL) is a rapidly progressing form of leukemia, characterized by the malignant transformation of B-lymphocytes. It primarily affects children, although adults can also develop this condition. As one of the most common hematologic cancers, B-cell ALL demands prompt diagnosis and a well-structured treatment approach to improve outcomes. In this article, we will delve into the specifics of B-cell acute lymphoblastic leukemia, examining its pathophysiology, risk factors, clinical presentation, diagnostic methods, and current treatment strategies.
Understanding B-cell Acute Lymphoblastic Leukemia
What is B-cell Acute Lymphoblastic Leukemia?
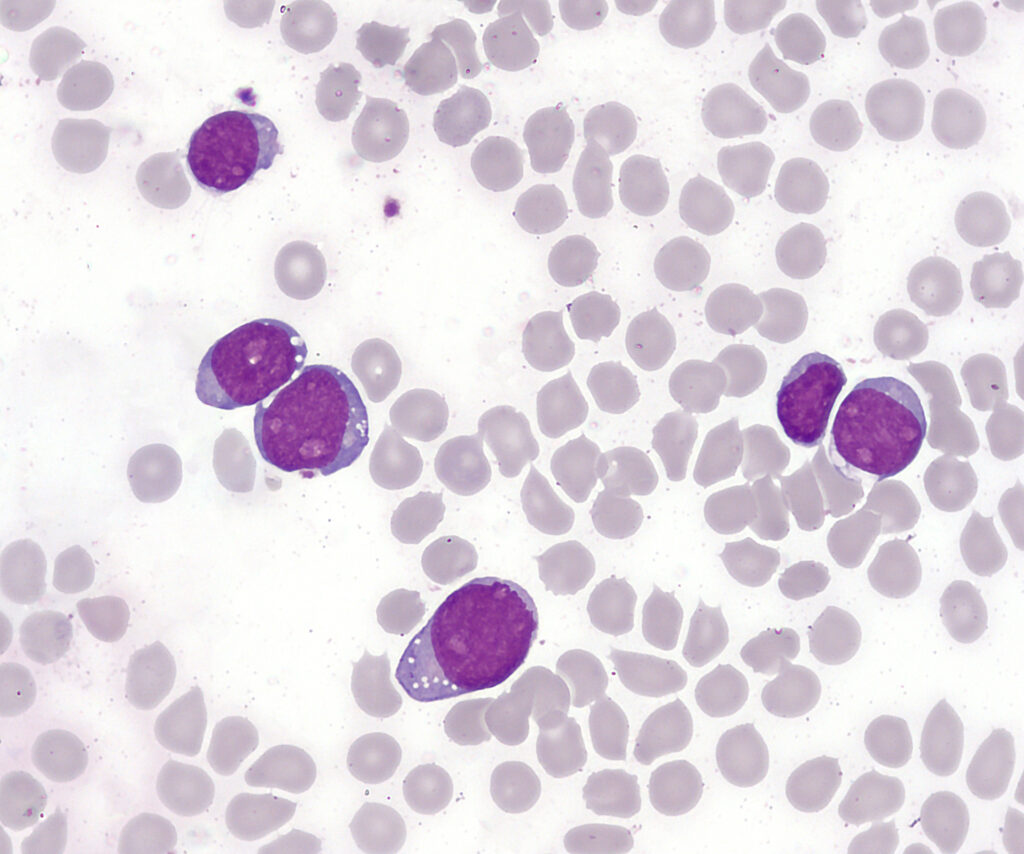
B-cell acute lymphoblastic leukemia (B-ALL) is a type of blood cancer that originates from immature white blood cells known as B-lymphocytes, which are a critical component of the immune system. These cells proliferate uncontrollably, crowding out normal blood cells, leading to various complications. B-ALL is classified as an acute leukemia, meaning it progresses rapidly and requires immediate medical intervention.
Pathophysiology of B-ALL
The pathophysiology of B-ALL involves genetic mutations that disrupt the normal development of B-lymphocytes. These mutations lead to the production of abnormal, immature white blood cells, which fail to function correctly and proliferate at an accelerated rate. The overproduction of these malignant cells leads to the infiltration of the bone marrow, lymph nodes, spleen, and other organs, contributing to a range of symptoms and complications.
Risk Factors for B-cell Acute Lymphoblastic Leukemia
While the exact cause of B-ALL remains unclear, several risk factors have been identified that may increase the likelihood of developing this condition. These include:
- Genetic predisposition: Children with certain genetic conditions, such as Down syndrome, are at a higher risk of developing B-ALL.
- Family history: A family history of leukemia or other cancers may increase the risk.
- Age: B-ALL most commonly affects children, especially those between the ages of 2 and 5.
- Exposure to radiation or chemotherapy: Previous exposure to high doses of radiation or certain chemotherapy drugs can increase the risk of leukemia.
- Environmental factors: Certain environmental factors, including exposure to chemicals such as benzene, may contribute to the development of B-ALL.
Clinical Presentation of B-cell Acute Lymphoblastic Leukemia
B-cell acute lymphoblastic leukemia presents with a wide range of symptoms, which can vary depending on the extent of disease spread and the organs involved. Common clinical manifestations include:
Common Symptoms
- Fatigue and weakness: Due to anemia caused by the infiltration of the bone marrow by leukemia cells.
- Fever: An early sign of infection due to a compromised immune system.
- Frequent infections: As a result of impaired white blood cell function.
- Pale skin: Caused by decreased red blood cell production.
- Bruising and bleeding: Low platelet counts can result in easy bruising, nosebleeds, or excessive bleeding from minor injuries.
- Bone pain: The infiltration of the bone marrow by leukemia cells can lead to bone pain.
- Enlarged lymph nodes, spleen, or liver: Abnormal cells may spread to these areas, causing noticeable swelling.
Pediatric-Specific Symptoms
In children, B-ALL may present with specific symptoms such as difficulty walking, bone or joint pain, and a general decline in physical activity due to fatigue and weakness.
Diagnosing B-cell Acute Lymphoblastic Leukemia
The diagnosis of B-cell acute lymphoblastic leukemia is confirmed through a combination of clinical evaluation, laboratory tests, and imaging studies.
Key Diagnostic Steps
- Complete blood count (CBC): This test helps identify abnormal levels of red blood cells, white blood cells, and platelets. A low red blood cell count (anemia), low platelet count (thrombocytopenia), and high or low white blood cell count may suggest leukemia.
- Bone marrow biopsy: A definitive diagnostic tool, where a sample of bone marrow is examined under a microscope for the presence of leukemia cells.
- Flow cytometry: This test helps identify the specific type of leukemia cells by detecting surface markers on the cells. In B-ALL, the leukemia cells are typically positive for CD19, CD22, and other B-cell markers.
- Cytogenetic analysis: This test examines the chromosomes in leukemia cells to identify specific genetic abnormalities that can provide information on prognosis and help guide treatment decisions.
Imaging Tests
- X-rays: To detect bone lesions or fractures associated with B-ALL.
- CT scans or ultrasounds: Used to assess the size of the spleen, liver, or lymph nodes.
Treatment Options for B-cell Acute Lymphoblastic Leukemia
The treatment of B-cell ALL is highly individualized, depending on factors such as the patient’s age, the presence of genetic mutations, and the severity of the disease. The goal is to achieve remission, reduce the risk of relapse, and cure the patient.
Chemotherapy
Chemotherapy is the cornerstone of B-ALL treatment. It is typically administered in phases:
- Induction therapy: The first phase aims to rapidly reduce the number of leukemia cells and induce remission. Common drugs include vincristine, prednisone, L-asparaginase, and daunorubicin.
- Consolidation therapy: This phase is intended to eliminate any remaining leukemia cells and reduce the risk of relapse. It may involve more intensive chemotherapy regimens.
- Maintenance therapy: A prolonged phase where lower doses of chemotherapy drugs are used to maintain remission and prevent relapse.
Targeted Therapy and Immunotherapy
Advances in targeted therapies have revolutionized the treatment of B-ALL. These therapies aim to specifically target cancer cells while sparing normal cells. Some key treatments include:
- Tyrosine kinase inhibitors: Such as imatinib, which is used in cases of B-ALL with the Philadelphia chromosome, a specific genetic abnormality.
- Monoclonal antibodies: Drugs like rituximab may be used to target and destroy leukemia cells.
- CAR-T cell therapy: Chimeric Antigen Receptor T-cell therapy involves modifying a patient’s T-cells to target B-cell leukemia cells. This cutting-edge treatment has shown promising results, especially in relapsed or refractory cases.
Stem Cell Transplantation
For patients at high risk of relapse or those who do not respond to initial chemotherapy, stem cell transplantation (also known as bone marrow transplantation) may be an option. This procedure involves replacing the patient’s diseased bone marrow with healthy stem cells from a donor.
Radiation Therapy
While not commonly used as a primary treatment, radiation therapy may be employed in certain cases to target specific areas, such as the brain or testicles, where leukemia cells are found.
Prognosis and Survival Rates
The prognosis for patients with B-cell ALL has improved significantly over the years, thanks to advancements in treatment. The survival rates vary depending on factors such as age, genetic abnormalities, and the response to initial treatment. For children with B-ALL, the five-year survival rate is approximately 85-90%. In contrast, adult patients tend to have a lower survival rate, though outcomes have improved with the introduction of targeted therapies.
Key Prognostic Factors:
- Age: Younger patients generally have a better prognosis.
- Genetic features: Certain genetic abnormalities, such as the Philadelphia chromosome, are associated with a worse prognosis, though targeted therapies can improve outcomes.
- Response to therapy: Early and complete remission is a strong predictor of long-term survival.
Managing B-cell Acute Lymphoblastic Leukemia: A Multidisciplinary Approach
The management of B-cell ALL requires a team of specialists, including oncologists, hematologists, radiologists, and pathologists. Additionally, supportive care is crucial in managing the side effects of treatment, such as infections, bleeding, and pain. Psychosocial support is also essential for patients and their families to cope with the emotional and psychological challenges associated with leukemia treatment.
B-cell acute lymphoblastic leukemia remains a challenging disease, but with advances in research and treatment, survival rates continue to improve. Early detection, personalized treatment regimens, and a multidisciplinary approach are key to achieving the best possible outcomes for patients. Ongoing research into targeted therapies and immunotherapies holds promise for further improving survival and reducing the side effects of treatment.