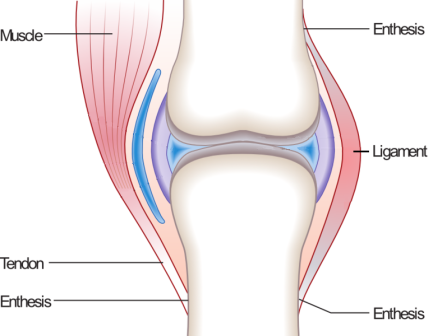
Enthesitis-related juvenile idiopathic arthritis (ERA-JIA) is a distinct subtype of juvenile idiopathic arthritis (JIA) that primarily affects the entheses—where tendons and ligaments attach to bones. It is a chronic autoimmune condition commonly diagnosed in children and adolescents, often linked to HLA-B27 genetic markers. This article delves into its symptoms, causes, diagnosis, and treatment strategies to provide a thorough understanding of the condition.
Symptoms of Enthesitis-Related Juvenile Idiopathic Arthritis
ERA-JIA manifests through a combination of musculoskeletal and systemic symptoms, including:
- Joint Pain and Swelling: Commonly affects large joints such as the knees, ankles, and hips.
- Enthesitis (Inflammation of Entheses): Pain and tenderness at ligament and tendon attachment points, particularly in the heels, knees, and lower back.
- Morning Stiffness: Reduced mobility, which improves with movement but can be persistent in advanced cases.
- Spinal Involvement: In some cases, inflammation may extend to the sacroiliac joints, leading to lower back pain.
- Fatigue and Generalized Malaise: Chronic inflammation can cause tiredness and decreased energy levels.
- Uveitis (Eye Inflammation): Some children may develop eye problems, including redness and vision disturbances.
Causes and Risk Factors
While the exact cause of ERA-JIA remains unclear, several genetic and environmental factors contribute to its development:
- Genetic Predisposition: The presence of the HLA-B27 gene increases susceptibility.
- Immune System Dysfunction: Abnormal immune responses trigger chronic inflammation.
- Environmental Triggers: Infections and other environmental exposures may play a role in disease onset.
- Sex and Age Factors: ERA-JIA is more common in boys and typically begins in late childhood or adolescence.
Diagnosis of ERA-JIA
Diagnosing ERA-JIA involves a combination of clinical evaluation, imaging studies, and laboratory tests:
Clinical Assessment
Physicians assess joint symptoms, enthesitis, and systemic manifestations. A history of prolonged joint pain and morning stiffness raises suspicion of ERA-JIA.
Laboratory Tests
- HLA-B27 Testing: Presence of this gene supports diagnosis but is not definitive.
- Inflammatory Markers: Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) indicate inflammation.
- Rheumatoid Factor (RF) and Anti-Nuclear Antibodies (ANA): Usually negative in ERA-JIA but help differentiate from other types of JIA.
Imaging Studies
- X-rays and MRI: Detect joint and sacroiliac inflammation, bone erosion, and structural changes.
- Ultrasound: Helps visualize enthesitis in early stages.
Treatment and Management Strategies
Management of ERA-JIA focuses on controlling inflammation, alleviating symptoms, and preventing long-term joint damage.
Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): First-line treatment to reduce pain and inflammation.
- Disease-Modifying Anti-Rheumatic Drugs (DMARDs): Methotrexate or sulfasalazine for more persistent cases.
- Biologic Therapies: TNF inhibitors (e.g., etanercept, adalimumab) for severe or refractory cases.
- Corticosteroids: Used sparingly for acute flare-ups.
Physical Therapy and Exercise
- Regular stretching and low-impact exercises maintain joint flexibility.
- Physiotherapy helps strengthen muscles and improve mobility.
- Hydrotherapy (water-based exercises) reduces joint strain.
Lifestyle and Supportive Care
- Maintaining a healthy weight reduces joint stress.
- Orthotic supports may help with foot and heel pain.
- Psychological support and counseling aid in coping with chronic illness.
Long-Term Outlook and Prognosis
ERA-JIA is a chronic condition, but early diagnosis and aggressive treatment improve long-term outcomes. While some children achieve remission, others may experience persistent symptoms into adulthood, sometimes progressing to ankylosing spondylitis. Regular monitoring by a pediatric rheumatologist is essential for disease management.