Enterococcus urinary tract infection caused by Enterococcus species, particularly Enterococcus faecalis and Enterococcus faecium, present a growing healthcare challenge due to their increasing antibiotic resistance. This article explores the causes, symptoms, diagnosis, treatment, and prevention of Enterococcus-related UTIs in detail.
What is Enterococcus?
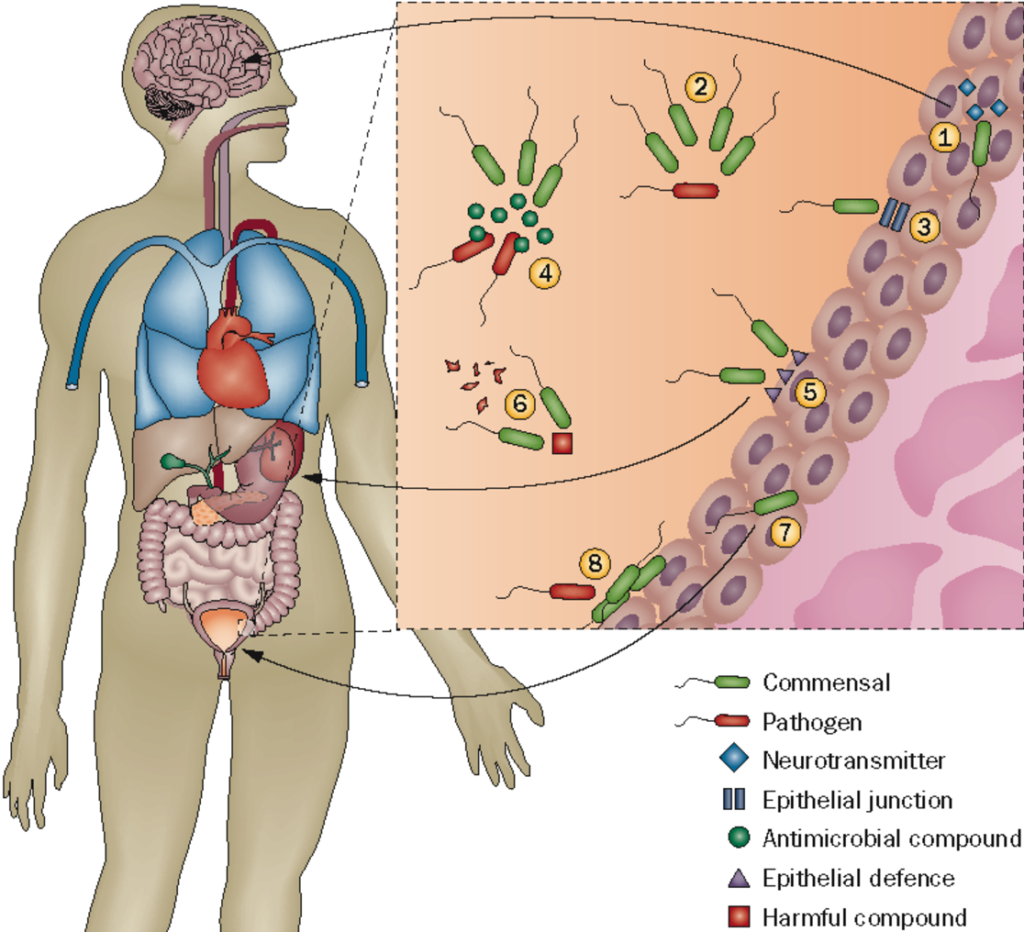
Enterococcus is a genus of Gram-positive bacteria commonly found in the human gastrointestinal tract. While typically harmless in healthy individuals, certain strains can become opportunistic pathogens, causing infections in the urinary tract, bloodstream, and other body sites.
Causes of Enterococcus UTI
1. Hospital-Acquired Infections
Patients with prolonged hospital stays, catheter use, or recent antibiotic treatment are at increased risk of Enterococcus UTIs.
2. Antibiotic Resistance
Enterococci, particularly E. faecium, have developed resistance to multiple antibiotics, including vancomycin (VRE), making infections harder to treat.
3. Weakened Immune System
Individuals with diabetes, cancer, or chronic illnesses are more susceptible to enterococcal infections.
4. Urinary Catheters and Medical Procedures
Use of indwelling catheters, prior surgeries, and urological procedures can introduce Enterococcus into the urinary tract.
Symptoms of Enterococcus UTI
- Frequent and painful urination (dysuria)
- Cloudy or foul-smelling urine
- Urgency and increased frequency of urination
- Lower abdominal or pelvic pain
- Blood in the urine (hematuria)
- Fever and chills (in severe cases, indicating possible kidney infection or sepsis)
Diagnosis of Enterococcus UTI
1. Urinalysis
A urine sample is analyzed for white blood cells (WBCs), red blood cells (RBCs), and bacteria.
2. Urine Culture and Sensitivity Test
A culture identifies the specific bacterial strain, while a sensitivity test determines antibiotic susceptibility.
3. Polymerase Chain Reaction (PCR) Testing
Molecular diagnostics can rapidly detect Enterococcus DNA in urine samples, especially in complicated or recurrent infections.
Treatment of Enterococcus UTI
1. Antibiotic Therapy
Treatment depends on the strain’s antibiotic susceptibility:
- Ampicillin: First-line treatment for susceptible Enterococcus infections.
- Vancomycin: Used for ampicillin-resistant strains but ineffective against vancomycin-resistant Enterococcus (VRE).
- Linezolid or Daptomycin: Used for VRE infections when other antibiotics fail.
2. Combination Therapy
For severe infections, a combination of aminoglycosides (e.g., gentamicin) with beta-lactams may be used for synergistic effects.
3. Symptomatic Treatment
- Increased fluid intake to flush bacteria from the urinary tract.
- Pain relievers (e.g., phenazopyridine) to ease discomfort.
4. Management of Recurrent Infections
- Prophylactic antibiotics for patients with frequent UTIs.
- Catheter management to reduce infection risk.
Prevention of Enterococcus UTI
1. Proper Hygiene Practices
- Regular handwashing and perineal hygiene can reduce bacterial spread.
2. Avoid Unnecessary Catheterization
- Minimize catheter use and follow strict aseptic techniques.
3. Stay Hydrated
- Drinking plenty of water helps flush out bacteria from the urinary system.
4. Strengthening the Immune System
- Maintain a healthy diet, manage chronic illnesses, and avoid excessive antibiotic use to prevent resistance.
Complications of Enterococcus UTI
If left untreated, Enterococcus UTIs can lead to severe complications:
- Pyelonephritis (kidney infection)
- Sepsis (life-threatening infection spread to the bloodstream)
- Chronic or recurrent infections leading to antibiotic resistance