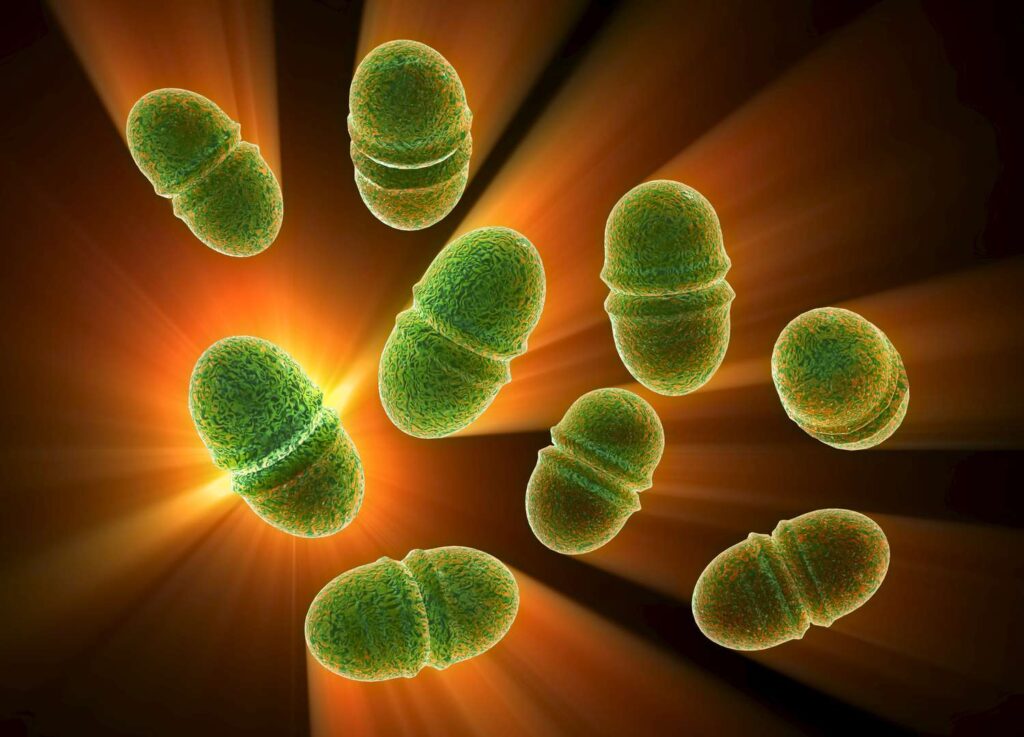
Enterococcus septicemia, also known as enterococcal bacteremia, is a serious bloodstream infection predominantly caused by Enterococcus faecalis and Enterococcus faecium. These Gram-positive, facultative anaerobic cocci are part of the normal gastrointestinal flora but can become opportunistic pathogens, especially in healthcare settings. The emergence of multidrug-resistant strains, particularly vancomycin-resistant enterococci (VRE), has complicated treatment protocols and heightened clinical concerns.
Etiology and Pathogenesis
Enterococcus species are resilient bacteria capable of surviving harsh conditions, including high salinity and a wide range of temperatures. Their intrinsic resistance to many antibiotics and ability to acquire additional resistance genes make them formidable pathogens. Infections typically arise from translocation of bacteria from the gastrointestinal tract or via contaminated medical devices. Virulence factors such as surface adhesins, biofilm formation, and secretion of enzymes like gelatinase contribute to their pathogenicity.
Risk Factors
Several factors predispose individuals to enterococcal septicemia:
- Healthcare Exposure: Prolonged hospital stays, especially in intensive care units, increase the risk of infection.
- Medical Devices: Use of indwelling catheters, central lines, and other invasive devices can serve as conduits for bacterial entry.
- Immunocompromised States: Patients with weakened immune systems, including those undergoing chemotherapy or organ transplantation, are more susceptible.
- Prior Antibiotic Use: Exposure to broad-spectrum antibiotics can disrupt normal flora, facilitating overgrowth and translocation of enterococci.
Clinical Manifestations
The presentation of enterococcal septicemia can vary but often includes:
- Fever and Chills: Common initial symptoms reflecting systemic infection.
- Hypotension: May progress to septic shock if not promptly managed.
- Organ Dysfunction: Depending on the infection’s severity and spread, organs such as the kidneys, liver, and lungs may be affected.
Diagnostic Approach
Accurate and timely diagnosis is crucial:
- Blood Cultures: Multiple sets are recommended to isolate and identify the causative organism.
- Antibiotic Susceptibility Testing: Determines the most effective antimicrobial therapy, especially important given the prevalence of resistant strains.
- Imaging Studies: May be warranted to identify potential sources or complications, such as abscesses or endocarditis.
Treatment Strategies
Management of enterococcal septicemia involves:
- Antibiotic Therapy: Guided by susceptibility results. Ampicillin remains effective against many E. faecalis strains, while E. faecium often requires alternative agents due to higher resistance rates. For VRE infections, options include linezolid or daptomycin.
- Combination Therapy: In severe cases, especially endocarditis, a combination of a cell wall–active agent (like ampicillin) with an aminoglycoside (such as gentamicin) may be employed to achieve synergistic bactericidal effects.
- Source Control: Removing or replacing contaminated devices and draining abscesses are essential steps in managing the infection.
Prevention Measures
Preventing enterococcal infections, particularly in healthcare settings, involves:
- Strict Adherence to Hand Hygiene: Proper handwashing protocols for healthcare workers to prevent cross-contamination.
- Judicious Antibiotic Use: Implementing antimicrobial stewardship programs to minimize unnecessary antibiotic exposure.
- Environmental Cleaning: Regular disinfection of surfaces and equipment to reduce the risk of nosocomial transmission.

