Tuberculosis (TB) remains a significant global health challenge, particularly in its active form, which is highly infectious and potentially life-threatening. Understanding active tuberculosis, its symptoms, diagnostic methods, and treatment strategies is essential to controlling its spread and ensuring patient recovery.
What Is Active Tuberculosis?
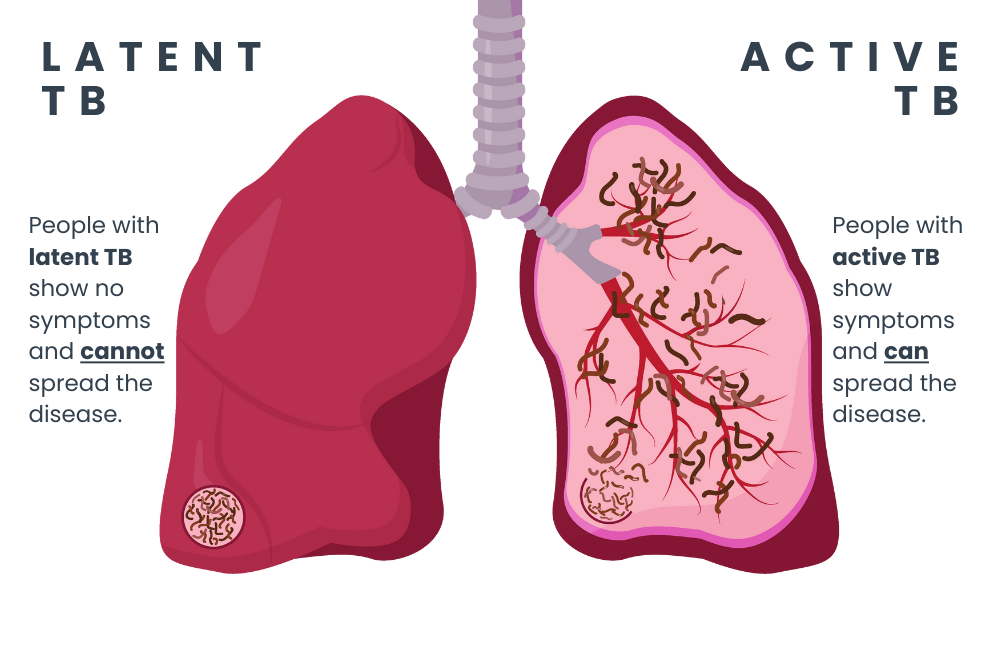
Active tuberculosis occurs when the Mycobacterium tuberculosis bacteria become active in the body and begin to multiply. Unlike latent TB, where the bacteria remain dormant and asymptomatic, active TB manifests with symptoms and poses a significant risk of transmission to others.
Key Characteristics of Active Tuberculosis
- Highly Infectious: Spread through airborne droplets from coughing, sneezing, or talking.
- Affects Lungs and Other Organs: Primarily impacts the lungs but can spread to other parts of the body, such as the lymph nodes, kidneys, or spine.
- Requires Immediate Treatment: Untreated active TB can lead to severe complications and death.
Symptoms of Active Tuberculosis
Active TB can present with a variety of symptoms, which may vary depending on the organ affected. Common symptoms include:
- Persistent Cough: Lasting three weeks or more, often producing phlegm or blood.
- Fever and Night Sweats: Indicating an active infection.
- Unintended Weight Loss: A hallmark symptom of advanced TB.
- Fatigue and Weakness: Resulting from the systemic effects of the infection.
- Chest Pain: Especially in cases involving pulmonary TB.
Extrapulmonary Tuberculosis Symptoms
In cases where TB spreads beyond the lungs, symptoms can vary widely:
- Lymph Node TB: Swelling of lymph nodes, often in the neck.
- Spinal TB: Back pain or stiffness.
- Renal TB: Blood in the urine and flank pain.
Causes and Transmission of Active Tuberculosis
TB is caused by the Mycobacterium tuberculosis bacterium, which spreads via airborne droplets. Key factors influencing transmission include:
- Prolonged Exposure: Close contact with an infected individual increases the risk.
- Weakened Immune System: Conditions such as HIV/AIDS, malnutrition, or diabetes can make individuals more susceptible.
- Overcrowded Environments: Poor ventilation and close quarters facilitate bacterial spread.
Diagnosis of Active Tuberculosis
Accurate and early diagnosis of active TB is critical for effective treatment. Common diagnostic methods include:
1. Chest X-Ray
- Helps identify abnormalities in the lungs, such as cavities or infiltrates.
2. Sputum Testing
- Microscopy: Detects acid-fast bacilli under a microscope.
- Culture: The gold standard for TB diagnosis, providing definitive identification of Mycobacterium tuberculosis.
3. Molecular Tests
- Rapid tests like GeneXpert detect TB bacteria and resistance to drugs like rifampin.
4. Tuberculin Skin Test (TST) or Interferon-Gamma Release Assay (IGRA)
- Useful for identifying latent TB but less specific for active disease.
Treatment for Active Tuberculosis
The treatment of active tuberculosis involves a combination of antibiotics over an extended period. Standard regimens ensure bacterial eradication while preventing drug resistance.
First-Line Drugs
- Isoniazid (INH): A cornerstone drug in TB treatment.
- Rifampin (RIF): Highly effective in killing TB bacteria.
- Pyrazinamide (PZA): Targets dormant bacteria in acidic environments.
- Ethambutol (EMB): Prevents bacterial resistance.
Treatment Duration
- Typically lasts 6–9 months, depending on the severity of the infection and patient adherence.
Drug-Resistant TB
For multidrug-resistant TB (MDR-TB), second-line drugs such as fluoroquinolones and injectable agents are used. Newer drugs like bedaquiline and delamanid are showing promise in treating resistant strains.
Preventing Active Tuberculosis
Vaccination
The Bacillus Calmette-Guérin (BCG) vaccine is effective in preventing severe TB forms in children. However, its efficacy in adults is limited.
Infection Control
- Isolation of Active Cases: Reduces the risk of transmission.
- Use of Masks: Prevents droplet spread.
- Improved Ventilation: Minimizes bacterial concentration in the air.
Regular Screening
High-risk individuals, such as healthcare workers or those with weakened immune systems, should undergo regular TB screenings to detect latent or active disease early.
Complications of Untreated Active Tuberculosis
Without treatment, active TB can lead to severe complications, including:
- Pulmonary Damage: Irreversible lung damage and respiratory failure.
- Miliary TB: Widespread infection affecting multiple organs.
- TB Meningitis: Inflammation of the membranes surrounding the brain.
Global Impact and TB Control Programs
Tuberculosis remains a major public health challenge worldwide. Initiatives like the WHO’s “End TB Strategy” aim to reduce TB incidence by improving access to diagnostics, treatment, and preventive care.
Active tuberculosis is a serious yet treatable condition. Prompt diagnosis, adherence to treatment regimens, and preventive measures are essential to controlling its spread and improving outcomes for affected individuals. By understanding its complexities, we can work towards a TB-free future.