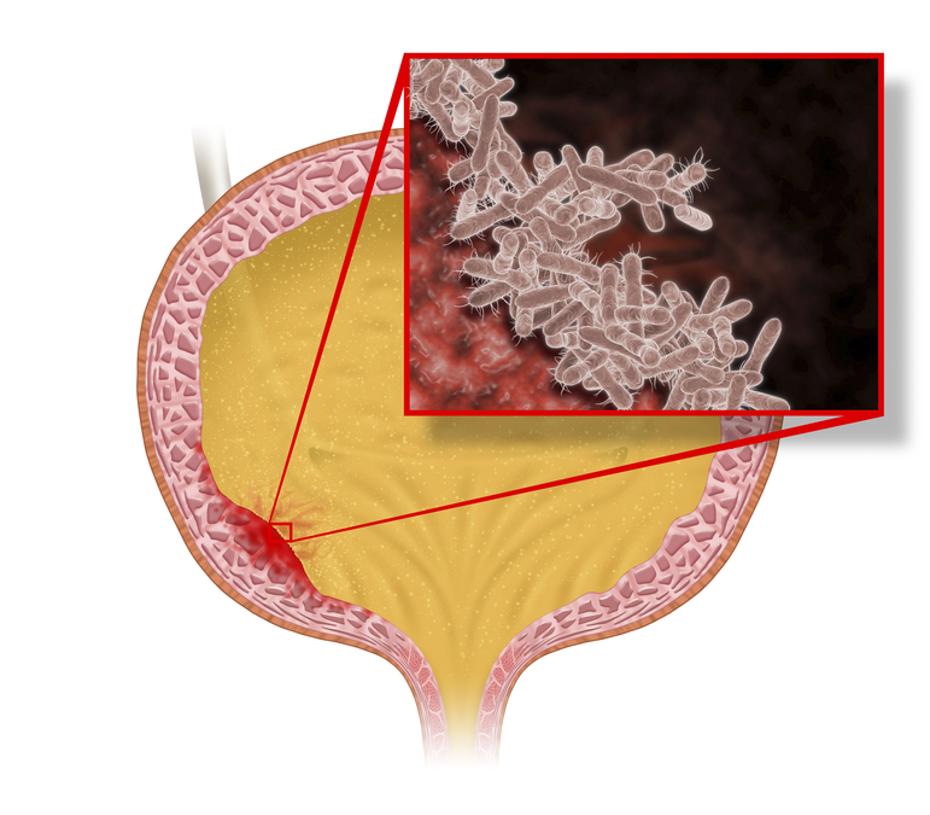
Enterococcus faecalis urinary tract infection faecalis is a gram-positive, facultatively anaerobic bacterium that naturally inhabits the gastrointestinal tract but can become pathogenic under certain conditions. It is one of the leading causes of urinary tract infections (UTIs), especially in hospitalized and immunocompromised patients. Due to its intrinsic and acquired resistance to various antibiotics, E. faecalis infections pose significant treatment challenges.
Causes and Risk Factors
How E. faecalis Causes UTIs
E. faecalis can enter the urinary tract through improper hygiene, catheter use, or invasive medical procedures. Once in the urinary system, the bacterium adheres to the urothelium and forms biofilms, enhancing its resistance to antibiotics and immune responses.
Key Risk Factors
- Hospitalization & Catheter Use: Indwelling catheters provide a direct entry path for E. faecalis.
- Weakened Immune System: Patients with diabetes, cancer, or organ transplants are at higher risk.
- Previous Antibiotic Use: Overuse of antibiotics can lead to resistant strains.
- Urinary Tract Abnormalities: Structural anomalies increase susceptibility.
- Elderly Patients: Aging weakens immune defenses and increases UTI frequency.
Symptoms of Enterococcus faecalis UTIs
- Frequent urination
- Burning sensation during urination (dysuria)
- Cloudy or bloody urine
- Foul-smelling urine
- Lower abdominal pain
- Fever and chills (in severe cases involving the kidneys)
Diagnosis
A proper diagnosis is essential for targeted treatment. Physicians use the following methods:
- Urine Culture: Confirms the presence of E. faecalis.
- Urinalysis: Detects white blood cells, red blood cells, and nitrites.
- Antibiotic Sensitivity Testing: Determines the most effective treatment option.
- Imaging (Ultrasound/CT Scan): Used in complicated or recurrent cases to identify structural abnormalities.
Treatment and Antibiotic Resistance
First-Line Antibiotics
- Ampicillin or Amoxicillin (preferred for susceptible strains)
- Nitrofurantoin (effective for lower UTIs but not for pyelonephritis)
- Fosfomycin (alternative option)
Antibiotic-Resistant Strains
- Vancomycin-resistant E. faecalis (VRE): Requires linezolid, daptomycin, or tigecycline.
- Combination Therapy: Beta-lactam with aminoglycosides may be required for severe infections.
Prevention Strategies
- Proper Hygiene: Wiping front to back reduces bacterial spread.
- Adequate Hydration: Flushes bacteria from the urinary system.
- Avoid Unnecessary Catheterization: Reduces infection risk.
- Cranberry Products: May help prevent bacterial adhesion.
- Probiotics: Help maintain healthy gut and urogenital flora.
Complications of E. faecalis UTI
- Pyelonephritis (Kidney Infection): Can lead to sepsis if untreated.
- Bacteremia and Endocarditis: Occurs when bacteria enter the bloodstream.
- Recurrent UTIs: Antibiotic resistance can make future infections harder to treat.