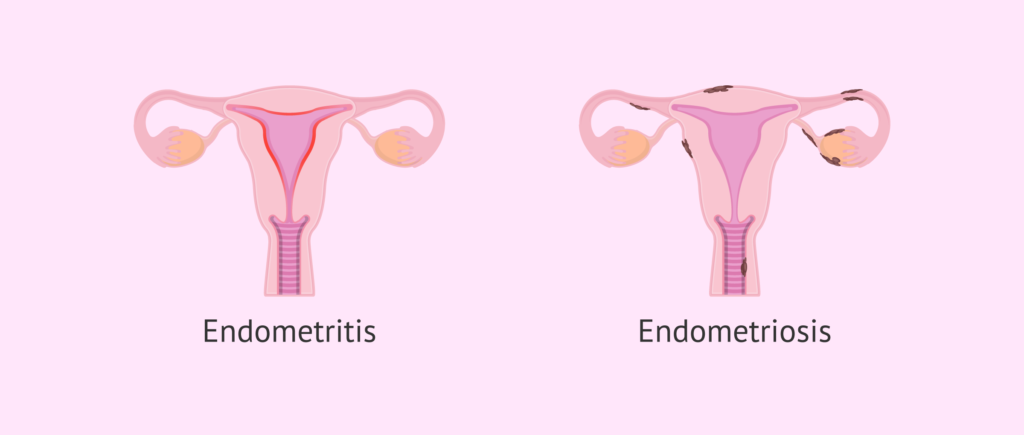
Endometritis is an inflammatory condition of the endometrial lining of the uterus, often caused by bacterial infections. One of the lesser-discussed but clinically significant pathogens involved in endometritis is Enterococcus species, primarily Enterococcus faecalis and Enterococcus faecium. These gram-positive cocci can cause persistent infections due to their ability to develop antibiotic resistance, making them a crucial concern in gynecological and obstetric care.
Causes and Risk Factors
Bacterial Invasion and Pathogenesis
Enterococcus species are part of the normal gastrointestinal and genitourinary flora but can become opportunistic pathogens under favorable conditions. They typically enter the uterine cavity through:
- Postpartum or post-abortion infections
- Gynecological surgeries, including cesarean sections and hysterectomies
- Prolonged use of intrauterine devices (IUDs)
- Pelvic inflammatory disease (PID)
- Immunosuppression or diabetes mellitus
- Prolonged antibiotic use leading to microbiome imbalance
Symptoms of Enterococcus Endometritis
The clinical presentation of enterococcal endometritis can range from mild to severe. Common symptoms include:
- Pelvic pain: Persistent lower abdominal discomfort
- Abnormal vaginal discharge: Foul-smelling or purulent secretions
- Fever and chills: Often indicative of a systemic inflammatory response
- Dysuria: Painful urination due to urethral involvement
- Menstrual irregularities: Heavy bleeding or spotting between cycles
Diagnosis of Enterococcus Endometritis
Early and accurate diagnosis is essential to prevent complications such as infertility or chronic pelvic pain. Diagnostic methods include:
1. Microbiological Culture and Sensitivity Testing
- Endometrial biopsy or cervical swabs are taken for bacterial culture.
- Gram staining reveals gram-positive cocci in pairs or chains.
- Antibiotic susceptibility testing helps determine the most effective treatment.
2. Blood Tests and Biomarkers
- Elevated white blood cell (WBC) count and C-reactive protein (CRP) levels suggest an ongoing infection.
3. Imaging Studies
- Transvaginal ultrasound may show endometrial thickening and inflammation.
- MRI or CT scans are reserved for severe cases with suspected abscess formation.
Treatment Strategies for Enterococcus Endometritis
1. Antibiotic Therapy
- First-line Treatment: Ampicillin or amoxicillin in combination with gentamicin.
- Resistant Strains: Vancomycin or linezolid may be required for vancomycin-resistant Enterococcus (VRE) infections.
- Oral vs. IV Administration: Severe cases require intravenous therapy, while mild cases may be managed with oral antibiotics.
2. Supportive Care
- Pain Management: NSAIDs or acetaminophen for symptom relief
- Hydration: Maintaining fluid balance to aid recovery
- Hospitalization: Required for severe infections with systemic involvement
3. Surgical Intervention
- Drainage of Abscesses: If pus accumulates within the uterus
- Hysterectomy: In extreme cases where the infection is recurrent and non-responsive to therapy
Prevention and Risk Reduction Strategies
- Strict Aseptic Techniques: During childbirth, gynecological procedures, and IUD insertions
- Antibiotic Stewardship: Judicious use of antibiotics to prevent resistance
- Regular Gynecological Check-ups: Early detection of infections and prompt treatment
- Proper Hygiene: Personal hygiene to minimize bacterial transfer