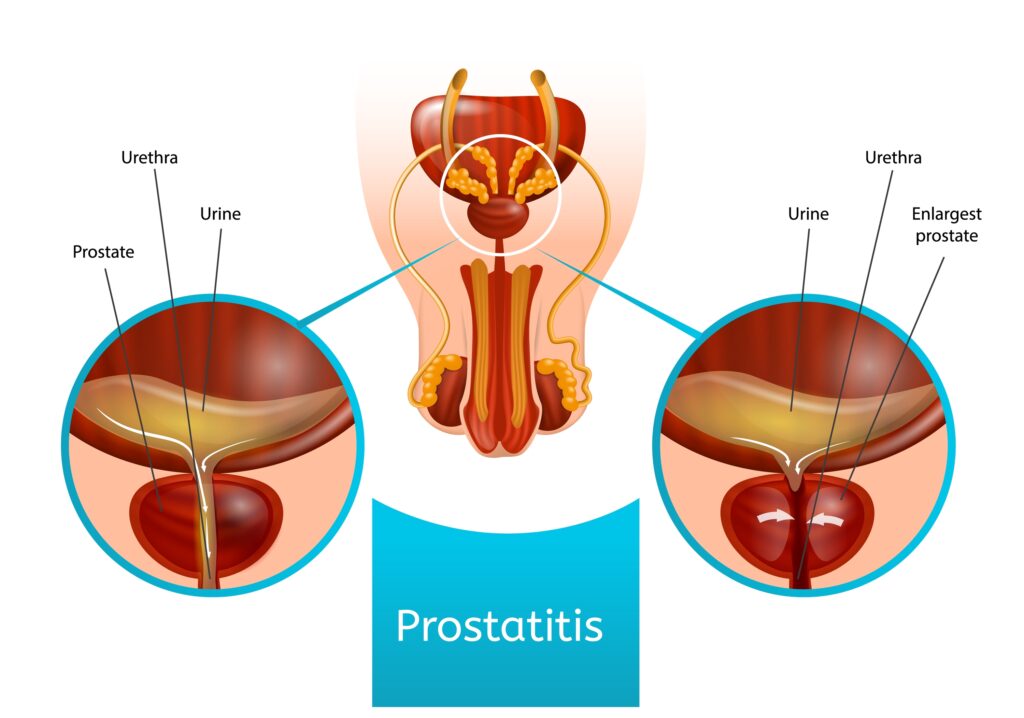
Enterobacter prostatitis is a bacterial infection of the prostate gland caused by Enterobacter species, a genus of Gram-negative bacteria commonly associated with urinary tract infections (UTIs) and hospital-acquired infections. While rare, Enterobacter prostatitis can lead to severe complications if left untreated. This article provides a comprehensive overview of the condition, including its causes, symptoms, diagnostic procedures, and treatment options.
Causes and Risk Factors
Bacterial Pathogenesis
Enterobacter species, particularly Enterobacter cloacae and Enterobacter aerogenes, are opportunistic pathogens that colonize the gastrointestinal and urinary tracts. They can infiltrate the prostate through the following pathways:
- Ascending Infection: Spread from an existing UTI
- Hematogenous Route: Bacteria enter the bloodstream and localize in the prostate
- Instrumentation: Catheterization, cystoscopy, or other invasive urological procedures
- Recurrent UTIs: Persistent infections increase the risk of bacterial prostatitis
Risk Factors
- Indwelling urinary catheters
- Prolonged antibiotic use leading to resistance
- Diabetes mellitus and immunosuppression
- Benign prostatic hyperplasia (BPH) or prostate surgery
- Sexually transmitted infections (STIs)
Symptoms and Clinical Presentation
Acute Enterobacter Prostatitis
- High fever and chills
- Pelvic or perineal pain
- Dysuria (painful urination)
- Urinary urgency and frequency
- Hematuria (blood in urine)
- Painful ejaculation
Chronic Enterobacter Prostatitis
- Persistent pelvic discomfort
- Recurrent UTIs
- Erectile dysfunction
- Intermittent low-grade fever
- Fatigue and malaise
Diagnosis
Laboratory Tests
- Urinalysis and Urine Culture: Identifies Enterobacter species in urine samples
- Prostatic Fluid Analysis: Expressed prostatic secretion (EPS) culture confirms bacterial presence
- Blood Tests: Elevated WBC count and inflammatory markers (CRP, ESR)
Imaging and Advanced Diagnostics
- Transrectal Ultrasound (TRUS): Detects abscess formation or structural abnormalities
- MRI or CT Scan: Useful in severe cases for abscess evaluation
- Urodynamic Studies: Assess urinary retention or obstruction
Treatment Options
Antibiotic Therapy
Empiric Therapy (Before Culture Results)
- Fluoroquinolones (e.g., Ciprofloxacin, Levofloxacin)
- Trimethoprim-Sulfamethoxazole (TMP-SMX)
Targeted Therapy (After Culture Sensitivity Testing)
- Carbapenems (e.g., Meropenem) for multidrug-resistant strains
- Cephalosporins (e.g., Cefepime) for susceptible strains
- Aminoglycosides (e.g., Gentamicin) in severe cases
Duration:
- Acute prostatitis: 4–6 weeks
- Chronic prostatitis: 6–12 weeks
Adjunct Therapies
- Alpha-blockers (Tamsulosin): Improve urinary flow
- NSAIDs: Reduce inflammation and pain
- Sitz Baths & Hydration: Promote comfort and flushing of bacteria
Complications
- Prostatic Abscess: Requires drainage
- Sepsis: Life-threatening systemic infection
- Chronic Bacterial Prostatitis: Long-term treatment challenges
- Antibiotic Resistance: Limits effective therapy options
Prevention Strategies
- Maintain proper urinary hygiene
- Avoid unnecessary catheterization
- Complete antibiotic courses to prevent resistance
- Monitor for recurrent UTIs in high-risk individuals