Enterobacter pneumoniais a serious bacterial infection caused by Enterobacter species, a group of gram-negative bacteria. These opportunistic pathogens are commonly associated with hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP), particularly in immunocompromised patients. Their inherent antibiotic resistance complicates treatment and increases morbidity and mortality rates. This article explores the causes, symptoms, diagnosis, and treatment strategies for Enterobacter pneumonia.
Causes and Risk Factors
1. Pathogenesis of Enterobacter Pneumonia
Enterobacter species, including Enterobacter cloacae and Enterobacter aerogenes, inhabit the gastrointestinal tract but can cause infections in compromised individuals. The infection often results from:
- Aspiration of colonized secretions from the oropharynx.
- Hematogenous spread from another infected site.
- Direct inoculation via mechanical ventilation or invasive procedures.
2. Risk Factors
Several factors predispose individuals to Enterobacter pneumonia, including:
- Hospitalization in intensive care units (ICUs)
- Mechanical ventilation and prolonged intubation
- Use of broad-spectrum antibiotics, leading to multidrug-resistant strains
- Weakened immune system, due to chemotherapy, diabetes, or HIV/AIDS
- Comorbidities, such as chronic lung disease, renal failure, or malignancies
Symptoms of Enterobacter Pneumonia
The clinical manifestations of Enterobacter pneumonia resemble other bacterial pneumonias but may be more severe. Common symptoms include:
- High fever and chills
- Persistent cough with purulent sputum
- Shortness of breath (dyspnea)
- Chest pain, often pleuritic in nature
- Increased respiratory rate (tachypnea)
- Altered mental status in elderly patients
Severe cases can lead to septic shock, acute respiratory distress syndrome (ARDS), and multi-organ failure.
Diagnosis
1. Clinical Evaluation
- Detailed medical history and physical examination to assess risk factors and symptoms.
2. Laboratory and Imaging Tests
- Blood cultures to detect systemic infection.
- Sputum culture and Gram stain to identify Enterobacter species.
- Bronchoalveolar lavage (BAL) in intubated patients.
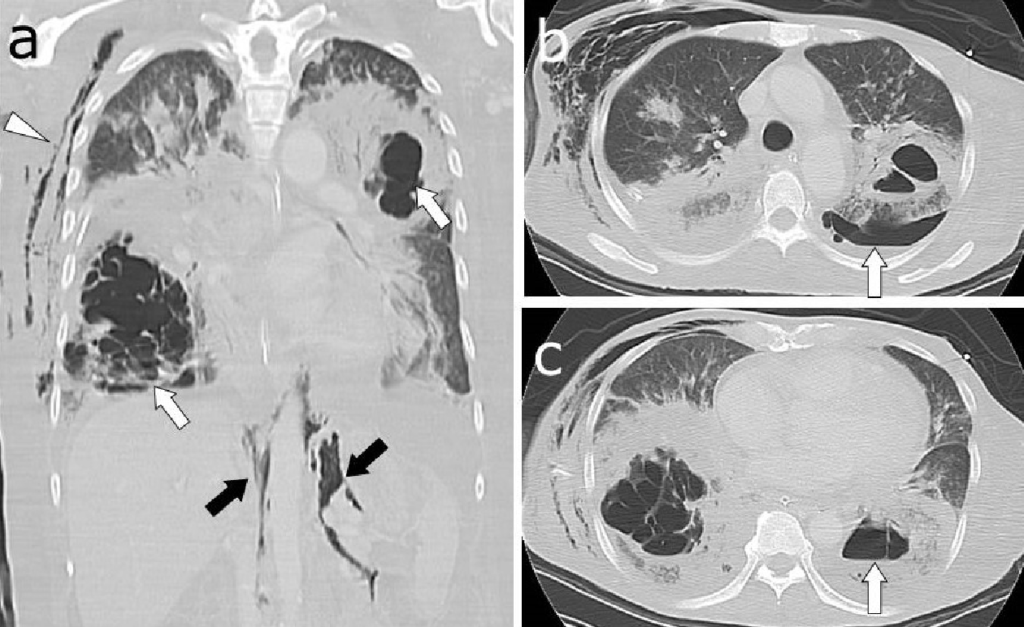
- Chest X-ray or CT scan to detect infiltrates, abscesses, or pleural effusions.
Treatment and Management
1. Empiric Antibiotic Therapy
Given the high antibiotic resistance of Enterobacter species, empiric treatment should include broad-spectrum antibiotics until culture results guide therapy.
- Carbapenems (e.g., meropenem, imipenem) for severe infections
- Piperacillin-tazobactam for less resistant strains
- Aminoglycosides (e.g., amikacin) as adjunct therapy
- Fluoroquinolones (e.g., levofloxacin) in selected cases
2. Definitive Treatment
Once antibiotic susceptibility is available, de-escalation to targeted therapy helps prevent resistance.
3. Supportive Care
- Oxygen therapy for respiratory distress
- Mechanical ventilation in severe cases
- Fluid management and vasopressors in septic shock
- Nutritional support for recovery
Prevention Strategies
1. Infection Control Measures
- Strict hand hygiene protocols in healthcare settings
- Proper disinfection of medical equipment
- Antibiotic stewardship programs to minimize resistance
2. Patient-Centered Prevention
- Early extubation in ventilated patients
- Head-of-bed elevation to prevent aspiration
- Regular oral care in ICU patients
Prognosis and Complications
Enterobacter pneumonia has a high mortality rate (20-50%), particularly in ICU patients. Complications include:
- Septicemia and bloodstream infections
- Pulmonary abscesses
- Respiratory failure requiring prolonged mechanical ventilation
- Multidrug resistance, leading to treatment failure