Enterobacter pelvic inflammatory disease is a significant infection of the female upper genital tract, encompassing the uterus, fallopian tubes, and ovaries. While commonly associated with sexually transmitted pathogens such as Neisseria gonorrhoeae and Chlamydia trachomatis, PID can also be instigated by other bacteria, including those from the Enterobacter genus. Understanding the role of Enterobacter species in PID is crucial for accurate diagnosis and effective treatment.
Etiology of Enterobacter-Induced PID
Enterobacter species are Gram-negative, facultatively anaerobic bacteria predominantly found in the gastrointestinal tract. These organisms can ascend from the lower genital tract to the upper reproductive organs, especially following procedures that disrupt the cervical barrier, such as endometrial biopsy, curettage, or hysteroscopy. The anatomical continuity of the female reproductive system facilitates this upward migration, leading to inflammation and infection.
Pathophysiology
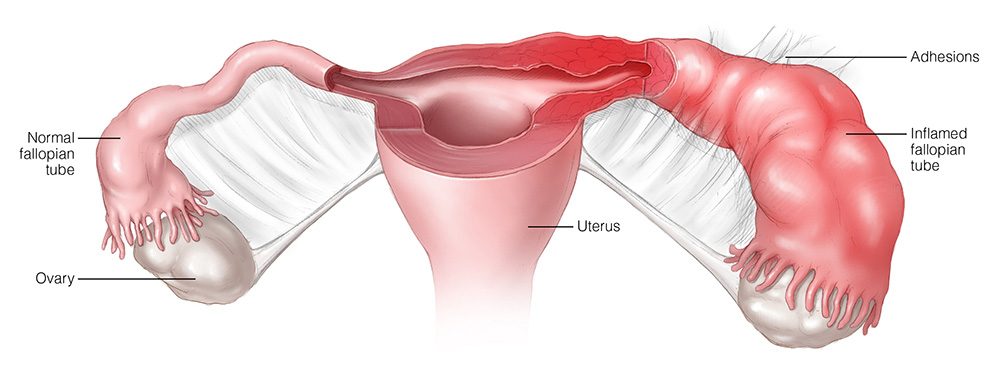
Once Enterobacter bacteria reach the upper genital tract, they trigger an inflammatory response. This inflammation can cause scarring, adhesions, and obstruction of the fallopian tubes, potentially leading to infertility or ectopic pregnancy. The loss of ciliated epithelial cells impairs ovum transport, further exacerbating reproductive complications.
Clinical Manifestations
The symptoms of PID caused by Enterobacter species are similar to those induced by other pathogens and may include:
- Lower abdominal or pelvic pain
- Abnormal vaginal discharge
- Fever and chills
- Pain during intercourse
- Irregular menstrual bleeding
- Painful or frequent urination
It’s important to note that some women may experience mild symptoms or be asymptomatic, underscoring the need for a high index of suspicion in at-risk populations.
Diagnosis
Diagnosing Enterobacter-induced PID involves a combination of clinical evaluation and laboratory testing:
- Clinical Examination: Assess for cervical motion tenderness, uterine tenderness, and adnexal tenderness.
- Microbiological Cultures: Obtain samples from the cervix, endometrium, or peritoneal fluid to identify Enterobacter species.
- Imaging Studies: Ultrasound or MRI may reveal tubo-ovarian abscesses or other pelvic abnormalities.
- Laboratory Tests: Elevated white blood cell count and inflammatory markers (e.g., C-reactive protein) support the diagnosis.
Treatment
Management of Enterobacter-related PID requires prompt and appropriate antibiotic therapy to prevent long-term sequelae:
- Antibiotic Regimen: Empirical broad-spectrum antibiotics should be initiated to cover Enterobacter species and other potential pathogens. Once culture results are available, therapy can be tailored accordingly.
- Hospitalization: Indicated for severe cases, pregnant patients, or when surgical intervention is necessary.
- Surgical Intervention: In cases of abscess formation or when there is no response to medical therapy, surgical drainage or removal of infected tissues may be required.
Prevention
Preventative measures are essential to reduce the incidence of PID:
- Safe Sexual Practices: Consistent use of condoms and limiting the number of sexual partners can decrease the risk of infection.
- Regular Medical Check-ups: Routine gynecological examinations and prompt treatment of lower genital tract infections can prevent the ascent of bacteria.
- Aseptic Techniques: Ensuring sterile conditions during gynecological procedures minimizes the risk of introducing Enterobacter species into the upper genital tract.

