Enterobacter meningitis is a rare but serious central nervous system (CNS) infection caused by Enterobacter species, a group of gram-negative, facultatively anaerobic bacilli. These bacteria are often nosocomial pathogens and can lead to life-threatening complications, particularly in neonates and immunocompromised patients.
Causes and Risk Factors
Enterobacter spp. are opportunistic pathogens that can colonize the gastrointestinal tract and spread through hematogenous dissemination or direct inoculation. Common risk factors include:
- Neonatal prematurity: Increased susceptibility due to immature immune defenses.
- Neurosurgical procedures: Ventriculoperitoneal shunts, external ventricular drains.
- Prolonged hospitalization: Intensive care unit (ICU) stays and mechanical ventilation.
- Immunosuppression: Cancer, HIV/AIDS, corticosteroid therapy.
- Head trauma: Open skull fractures and post-surgical infections.
Pathophysiology
Enterobacter species produce a variety of virulence factors, including:
- Capsular polysaccharides: Resist host immune defenses.
- Adhesins: Facilitate colonization of the meninges.
- Beta-lactamases: Confer resistance to broad-spectrum antibiotics.
- Lipopolysaccharides (LPS): Trigger severe inflammatory responses leading to neuronal damage.
graph TD;
A[Enterobacter spp.] -->|Colonization| B[Gastrointestinal Tract];
B -->|Hematogenous Spread| C[Bloodstream];
C -->|Blood-Brain Barrier Penetration| D[Meninges];
D -->|Inflammation & Neuronal Damage| E[Severe CNS Complications];Clinical Presentation
Symptoms of Enterobacter meningitis vary depending on age and immune status:
Neonates
- Fever or hypothermia
- Lethargy, irritability, poor feeding
- Bulging fontanelle
- Seizures
- Respiratory distress
Adults and Immunocompromised Patients
- Fever, headache
- Neck stiffness (nuchal rigidity)
- Altered mental status, confusion
- Seizures
- Photophobia and vomiting
Diagnosis
Early and accurate diagnosis is critical for effective treatment. Diagnostic procedures include:
- Lumbar puncture (CSF analysis): Increased white blood cell count, elevated protein, decreased glucose levels.
- Gram staining & culture: Identification of gram-negative rods.
- Polymerase chain reaction (PCR): Rapid pathogen detection.
- Blood cultures: Confirm systemic infection.
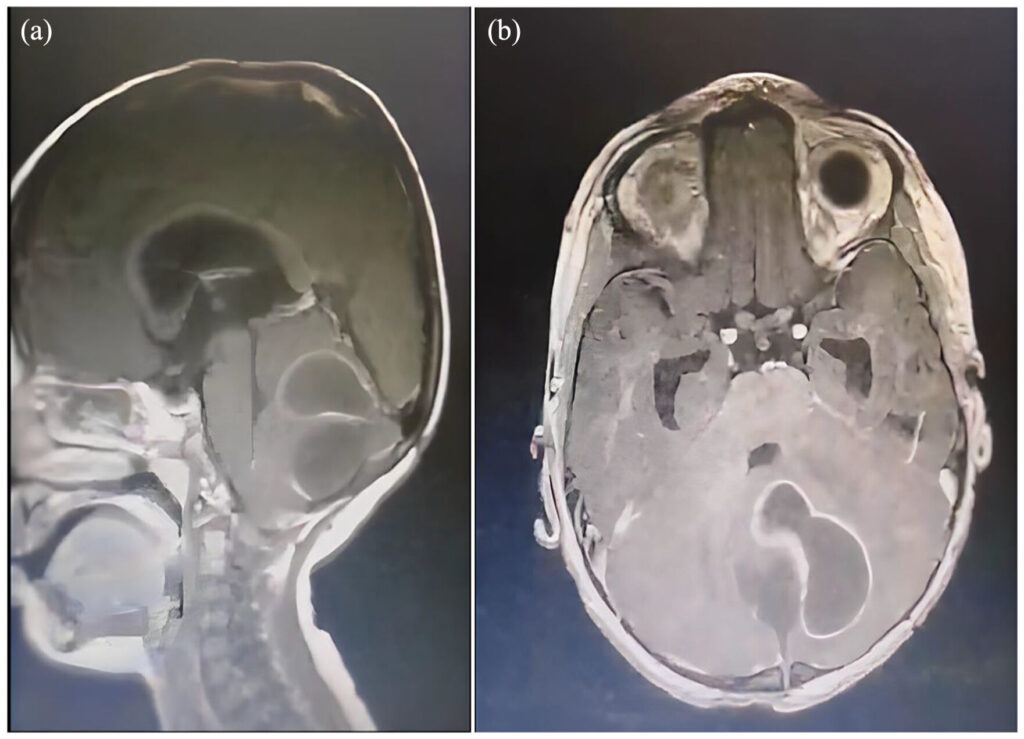
- Neuroimaging (CT/MRI): Identify complications such as hydrocephalus or abscess formation.
Treatment Strategies
Management involves prompt initiation of antimicrobial therapy and supportive care.
Empirical Antibiotic Therapy
Given the high antibiotic resistance of Enterobacter spp., treatment often requires combination therapy:
- Carbapenems (e.g., meropenem, imipenem): Broad-spectrum coverage.
- Cefepime or Ceftazidime: Extended-spectrum cephalosporins.
- Aminoglycosides (e.g., amikacin, gentamicin): Synergistic bactericidal effect.
- Polymyxins (e.g., colistin): For multidrug-resistant (MDR) strains.
Adjunctive Therapy
- Dexamethasone: Reduces inflammation and neuronal damage.
- Intrathecal antibiotics: Used in refractory cases.
- Supportive care: Fluid management, seizure control, and respiratory support.
Prognosis and Complications
Mortality and morbidity depend on early diagnosis and appropriate treatment. Possible complications include:
- Hydrocephalus: CSF obstruction requiring shunting.
- Cerebral abscess: Localized infection needing surgical drainage.
- Seizure disorders: Long-term neurological sequelae.
- Hearing loss: Due to CNS inflammation affecting the auditory nerve.
Prevention Strategies
- Strict aseptic techniques: During neurosurgical procedures and catheter placements.
- Antibiotic stewardship: Avoid unnecessary antibiotic use to limit resistance.
- Hand hygiene and infection control: Reduce hospital-acquired infections.
- Vaccination: Though no specific vaccine exists for Enterobacter, general meningitis vaccines (Hib, pneumococcal, meningococcal) reduce overall risk.

