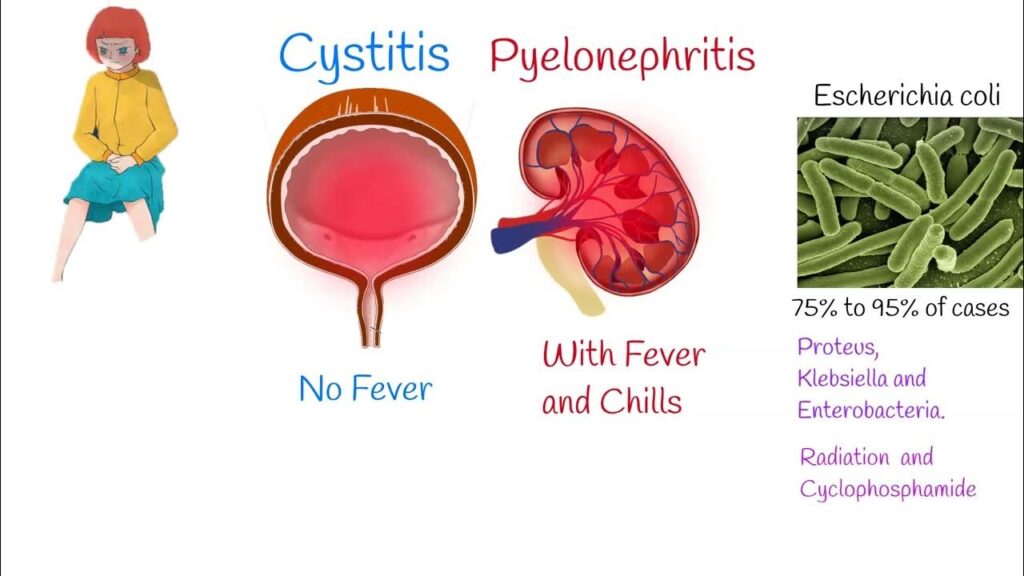
Enterobacter cystitis is a urinary tract infection (UTI) caused by bacteria of the Enterobacter genus. These gram-negative, facultatively anaerobic bacilli are part of the Enterobacteriaceae family and are commonly found in the gastrointestinal tract. While they are typically harmless, certain conditions can lead to their proliferation in the urinary system, resulting in cystitis.
Etiology and Risk Factors
Enterobacter species are opportunistic pathogens. Infections often arise in healthcare settings, particularly among individuals with weakened immune systems or those with indwelling medical devices. Key risk factors include:
- Hospitalization: Prolonged stays increase exposure to nosocomial pathogens.
- Catheterization: Indwelling urinary catheters can introduce bacteria into the bladder.
- Immunosuppression: Conditions like diabetes or treatments such as chemotherapy can compromise immune defenses.
- Prior Antibiotic Use: Broad-spectrum antibiotics can disrupt normal flora, facilitating Enterobacter overgrowth.
Pathophysiology
The pathogenesis of Enterobacter cystitis involves the bacteria’s ability to adhere to and invade the urothelium. Virulence factors such as adhesins and lipopolysaccharide capsules enable the bacteria to evade host defenses and establish infection. The presence of beta-lactamases contributes to antibiotic resistance, complicating treatment.
Clinical Manifestations
Symptoms of Enterobacter cystitis are similar to those of other bacterial UTIs and may include:
- Dysuria (painful urination)
- Increased urinary frequency and urgency
- Suprapubic discomfort
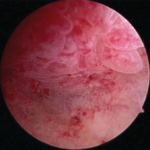
- Hematuria (blood in the urine)
- Fever and malaise in more severe cases
Diagnostic Evaluation
Accurate diagnosis involves:
- Urine Analysis: Detection of pyuria and bacteriuria.
- Urine Culture: Isolation and identification of Enterobacter species.
- Antibiotic Sensitivity Testing: Determining the susceptibility profile to guide therapy.
Treatment Strategies
Management of Enterobacter cystitis requires targeted antibiotic therapy, considering the organism’s resistance patterns. Empirical treatment may involve carbapenems or fourth-generation cephalosporins, but therapy should be adjusted based on culture results. Removal or replacement of indwelling catheters is essential to prevent recurrence.
Prevention Measures
Preventive strategies focus on reducing risk factors:
- Aseptic Techniques: Strict adherence during catheter insertion and maintenance.
- Judicious Antibiotic Use: To minimize the development of resistant strains.
- Monitoring and Early Intervention: Regular assessment of patients with catheters or those in intensive care units.