Complicated urinary tract infections (UTIs) represent a significant clinical challenge, particularly when caused by opportunistic pathogens such as Enterobacter species. These infections often arise in patients with underlying health conditions or anatomical abnormalities, leading to increased morbidity and a heightened risk of treatment failure. Understanding the unique characteristics of Enterobacter-induced complicated UTIs is essential for effective diagnosis and management.
Etiology and Pathophysiology
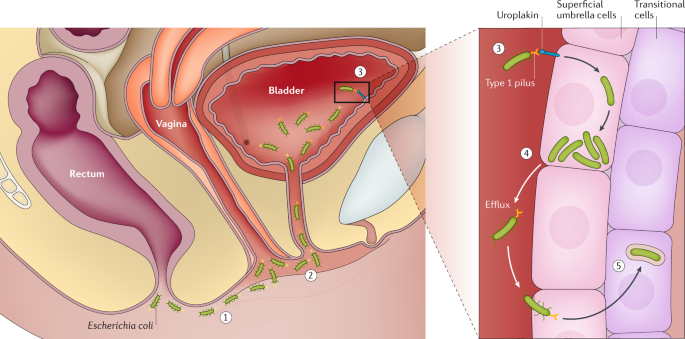
Enterobacter species are Gram-negative, facultative anaerobic bacilli belonging to the Enterobacteriaceae family. Commonly found in the gastrointestinal tract, these organisms can become pathogenic, especially in healthcare settings. Their ability to form biofilms and acquire resistance genes complicates treatment strategies.
The pathogenesis of Enterobacter-related UTIs involves the bacteria ascending the urinary tract, adhering to uroepithelial cells, and evading host immune responses. Biofilm formation on indwelling medical devices, such as catheters, provides a protective environment against both the host’s defenses and antimicrobial agents, leading to persistent infections.
Risk Factors
Several factors predispose individuals to complicated UTIs caused by Enterobacter species:
- Hospitalization: Prolonged stays increase exposure to nosocomial pathogens.
- Indwelling Urinary Catheters: Serve as a surface for biofilm formation and bacterial colonization.
- Immunosuppression: Conditions such as diabetes mellitus, malignancies, or immunosuppressive therapies diminish the body’s ability to combat infections.
- Structural Abnormalities: Anomalies like urinary obstructions or neurogenic bladder impede normal urine flow, facilitating bacterial growth.
- Prior Antibiotic Use: Previous exposure, especially to broad-spectrum antibiotics, can disrupt normal flora and select for resistant Enterobacter strains.
Clinical Presentation
The symptoms of complicated UTIs are often more severe than those of uncomplicated infections and may include:
- Lower Urinary Tract Symptoms: Dysuria, urgency, frequency, and suprapubic discomfort.
- Systemic Manifestations: Fever, chills, flank pain, and signs of sepsis in severe cases.
- Laboratory Findings: Pyuria, hematuria, and the presence of Enterobacter species in urine cultures.
Diagnostic Approach
Accurate diagnosis involves a combination of clinical assessment and laboratory investigations:
- Urine Analysis and Culture: Microscopic examination and culture to identify the causative organism and determine antibiotic susceptibility.
- Blood Cultures: Recommended if systemic infection or sepsis is suspected.
- Imaging Studies: Ultrasound or computed tomography (CT) scans to detect anatomical abnormalities, abscesses, or obstructions.
Treatment Strategies
Managing Enterobacter-induced complicated UTIs requires a multifaceted approach:
- Antimicrobial Therapy: Empirical treatment should be guided by local resistance patterns, with adjustments made based on culture results. Enterobacter species often exhibit resistance to multiple antibiotics due to inducible beta-lactamases. Carbapenems have been the mainstay of treatment; however, emerging resistance necessitates alternative options.
- Cefiderocol: A siderophore cephalosporin effective against multidrug-resistant Gram-negative bacteria, including carbapenem-resistant Enterobacteriaceae. It utilizes a unique mechanism, hijacking bacterial iron transport systems to gain entry into the cell.
- Aztreonam/Avibactam: This combination pairs a monobactam with a beta-lactamase inhibitor, targeting metallo-beta-lactamase-producing strains. Approved in the European Union in 2024, it offers a viable option against resistant infections.
- Meropenem/Vaborbactam: Combines a carbapenem with a novel beta-lactamase inhibitor, restoring activity against certain carbapenemase-producing organisms. Approved for medical use in the United States in 2017, it addresses infections caused by resistant Enterobacter strains.
- Source Control: Removing or replacing infected indwelling devices and addressing any anatomical abnormalities to prevent recurrence.
- Supportive Care: Ensuring adequate hydration, pain management, and monitoring for potential complications.
Prevention Measures
Preventing Enterobacter-related complicated UTIs involves:
- Strict Adherence to Aseptic Techniques: During catheter insertion and maintenance to minimize infection risk.
- Judicious Antibiotic Use: To reduce the development of resistant strains.
- Regular Surveillance: Monitoring for signs of infection, especially in high-risk populations.