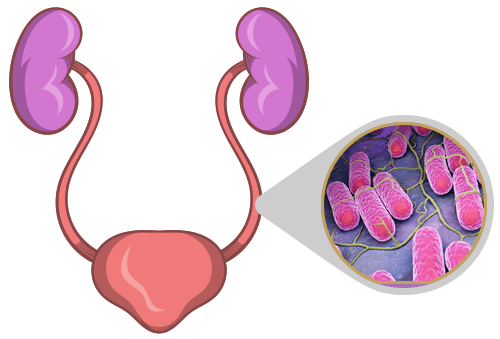
Enterobacter cloacae is a facultatively anaerobic, Gram-negative bacterium that naturally resides in the gastrointestinal tract. While generally harmless in healthy individuals, it can become pathogenic, particularly in hospital settings, leading to urinary tract infections (UTIs). These infections are often complicated by antibiotic resistance, making their management a significant challenge. This article provides an in-depth analysis of Enterobacter cloacae UTIs, their causes, symptoms, diagnosis, treatment, and prevention.
Causes and Risk Factors
Hospital and Healthcare-Associated Infections
Enterobacter cloacae is a major cause of nosocomial infections, meaning it is commonly acquired in hospitals and healthcare settings. Risk factors include:
- Prolonged hospitalization
- Use of urinary catheters (CAUTIs)
- Immunosuppression (e.g., chemotherapy, organ transplants, diabetes, or HIV/AIDS)
- Prior antibiotic use, leading to multidrug resistance
- Surgical procedures involving the urinary tract
- Chronic kidney disease or dialysis
Community-Acquired Infections
Although less common, Enterobacter cloacae can cause UTIs in community settings, often due to:
- Poor hygiene and inadequate hydration
- Unprotected sexual activity
- Recurrent UTIs with inappropriate antibiotic treatment
Symptoms of Enterobacter cloacae UTI
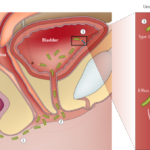
The symptoms of an Enterobacter cloacae urinary tract infection vary depending on the severity and location of the infection.
Lower UTI (Cystitis) Symptoms:
- Frequent and painful urination (dysuria)
- Urgency and increased urination frequency
- Hematuria (blood in urine)
- Cloudy or foul-smelling urine
- Mild lower abdominal discomfort
Upper UTI (Pyelonephritis) Symptoms:
- Fever and chills
- Flank pain (pain on the side of the abdomen or back)
- Nausea and vomiting
- Severe fatigue and weakness
In immunocompromised individuals, the infection can progress rapidly and lead to urosepsis, a life-threatening condition requiring urgent medical intervention.
Diagnosis of Enterobacter cloacae UTI
1. Urinalysis and Urine Culture
- Urine dipstick test detects leukocytes and nitrites, indicating bacterial infection.
- Urine culture confirms the presence of Enterobacter cloacae and guides antibiotic selection.
2. Antibiotic Susceptibility Testing (AST)
- Determines resistance patterns, crucial for effective treatment due to multidrug-resistant strains.
3. Blood Tests and Imaging
- Complete blood count (CBC) to assess infection severity.
- Renal ultrasound or CT scan in suspected upper UTI cases.
Treatment of Enterobacter cloacae UTI
First-Line Antibiotic Therapy
- Carbapenems (e.g., meropenem, imipenem) – Preferred for severe infections due to multidrug resistance.
- Fluoroquinolones (e.g., ciprofloxacin, levofloxacin) – Often used in non-resistant cases.
- Aminoglycosides (e.g., gentamicin, amikacin) – Used in combination therapy for complicated UTIs.
Multidrug-Resistant Enterobacter cloacae UTI Treatment
In cases of Extended-Spectrum Beta-Lactamase (ESBL)-producing or Carbapenem-Resistant Enterobacter cloacae (CRE):
- Colistin or polymyxins may be used as a last resort.
- Combination therapy with fosfomycin or tigecycline in severe cases.
Supportive Care
- Increased fluid intake to flush bacteria.
- Pain relievers (e.g., acetaminophen for fever and discomfort).
Prevention Strategies
Hospital Infection Control Measures
- Strict catheter management protocols (early removal, sterile insertion).
- Hand hygiene compliance among healthcare workers.
- Antibiotic stewardship programs to reduce resistance.
Personal Preventive Measures
- Stay hydrated to promote urine flow and flush out bacteria.
- Practice good hygiene, especially after using the restroom.
- Avoid unnecessary antibiotic use to prevent resistance.
- Urinate after sexual activity to reduce bacterial transfer.
Complications of Enterobacter cloacae UTI
If left untreated, an Enterobacter cloacae UTI can lead to severe complications:
- Pyelonephritis – Infection spreading to the kidneys.
- Urosepsis – Systemic infection leading to organ failure.
- Renal abscesses – Pockets of pus in the kidney.
- Chronic UTI recurrence – Persistent infections due to antibiotic resistance.