Enterobacter cloacae is a Gram-negative, facultative anaerobic bacterium that commonly inhabits the human gastrointestinal tract. While typically a commensal organism, it can act as an opportunistic pathogen, causing severe infections, particularly in hospitalized patients. Among these, bronchitis caused by Enterobacter cloacae is a serious concern, often linked to antibiotic resistance and nosocomial infections.
This article provides an in-depth examination of Enterobacter cloacae bronchitis, including its causes, risk factors, clinical manifestations, diagnostic approaches, and the latest treatment strategies.
Understanding Enterobacter cloacae in Bronchitis
Pathophysiology and Virulence Factors
Enterobacter cloacae possesses several virulence mechanisms that enable it to colonize and infect the respiratory tract:
- Adhesion Factors: Facilitates attachment to bronchial epithelial cells.
- Biofilm Formation: Enhances bacterial survival and resistance to antibiotics.
- Beta-Lactamase Production: Inactivates beta-lactam antibiotics, leading to multidrug resistance (MDR).
- Lipid A and Lipopolysaccharide (LPS): Triggers inflammation and immune evasion.
Once in the respiratory tract, these factors contribute to bronchial inflammation, mucus hypersecretion, and airway obstruction, hallmarks of bronchitis.
Risk Factors for Enterobacter cloacae Bronchitis
Certain conditions predispose individuals to developing bronchitis due to Enterobacter cloacae:
- Hospitalization and ICU Stay – Particularly with mechanical ventilation.
- Chronic Respiratory Diseases – COPD, asthma, and bronchiectasis increase susceptibility.
- Immunocompromised States – Cancer, organ transplantation, HIV/AIDS, or long-term corticosteroid use.
- Prolonged Antibiotic Use – Alters normal flora, promoting resistant bacterial overgrowth.
- Invasive Medical Devices – Endotracheal tubes, ventilators, and bronchoscopy procedures create entry points for infection.
These factors not only increase the risk of bronchitis but also complicate treatment due to the bacterium’s resistance profile.
Clinical Manifestations of Enterobacter cloacae Bronchitis
Symptoms of E. cloacae-induced bronchitis can resemble other bacterial respiratory infections:
- Persistent productive cough with thick, purulent sputum.
- Shortness of breath (dyspnea) and increased respiratory effort.
- Fever and chills, often indicative of systemic involvement.
- Chest discomfort or pain due to airway inflammation.
- Wheezing and rales on auscultation, suggesting bronchial obstruction.
In severe cases, bronchopneumonia may develop, leading to acute respiratory distress syndrome (ARDS).
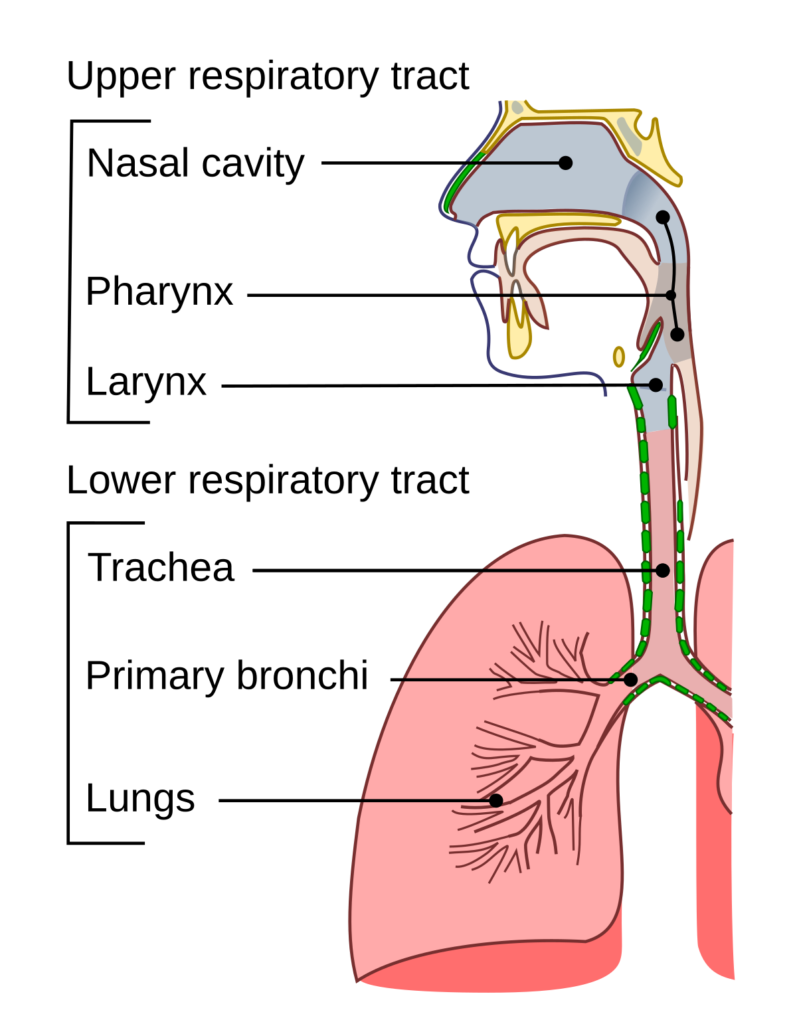
Diagnostic Approaches
1. Microbiological Identification
- Sputum Culture & Gram Stain: Confirms the presence of Gram-negative rods.
- Bronchoalveolar Lavage (BAL): Recommended for ventilated patients to obtain lower respiratory secretions.
2. Molecular and Biochemical Tests
- PCR Assays: Detect Enterobacter species with high specificity.
- MALDI-TOF Mass Spectrometry: Rapid bacterial identification.
3. Antibiotic Susceptibility Testing (AST)
- Disk Diffusion and MIC Determination: Identifies resistance patterns (e.g., ESBL, carbapenemase production).
4. Imaging Studies
- Chest X-ray: May reveal peribronchial thickening or infiltrates.
- CT Scan: Provides more detailed imaging, especially in complicated cases.
Treatment Strategies
1. Empirical Antibiotic Therapy
Given its high antibiotic resistance, initial treatment must cover multi-drug-resistant (MDR) Enterobacter cloacae.
- First-line Choices (Before AST Results):
- Carbapenems (Meropenem, Imipenem) – Preferred for ESBL-producing strains.
- Piperacillin-Tazobactam – Effective against non-ESBL-producing strains.
- Aminoglycosides (Gentamicin, Amikacin) – Used in combination therapy.
2. Targeted Therapy (After AST Results)
Once susceptibility testing is available, de-escalation to a narrower-spectrum antibiotic is advised to minimize resistance:
- If Carbapenem-Resistant: Polymyxins (Colistin) or Tigecycline.
- If ESBL-Negative: Third-generation cephalosporins (Ceftriaxone, Cefotaxime).
3. Supportive Care
- Oxygen Therapy: For hypoxia in severe cases.
- Bronchodilators: Improve airflow in obstructive symptoms.
- Mucolytics: Help clear thick bronchial secretions.
Prevention of Enterobacter cloacae Respiratory Infections
1. Infection Control in Healthcare Settings
- Hand Hygiene Compliance: Reduces nosocomial transmission.
- Proper Ventilator Management: Reduces the incidence of ventilator-associated pneumonia (VAP).
- Contact Precautions: Isolation of patients with MDR strains.
2. Antimicrobial Stewardship
- Rational Antibiotic Prescribing: Minimizes resistance development.
- De-escalation Strategies: Optimize treatment duration and spectrum.
3. Immunization & Respiratory Health Maintenance
- Pneumococcal & Influenza Vaccination: Reduces co-infections.
- Smoking Cessation: Lowers bronchial inflammation risk.