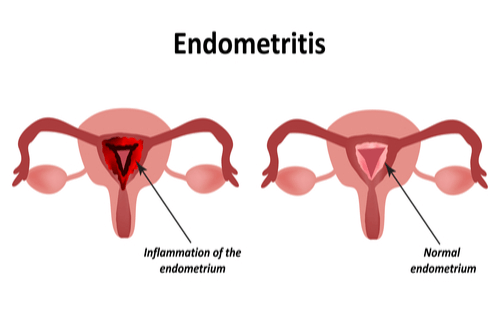
Endometritis refers to the inflammation of the endometrium, the inner lining of the uterus. This condition arises primarily due to infections and can manifest in acute or chronic forms. Prompt recognition and treatment are essential to prevent complications, including fertility issues.
Causes of Endometritis
Endometritis is predominantly caused by bacterial infections. Common pathogens include:
- Sexually Transmitted Infections (STIs): Chlamydia trachomatis and Neisseria gonorrhoeae are frequent culprits.
- Postpartum Infections: Bacteria from the vaginal flora can ascend into the uterus during childbirth, especially after prolonged labor or cesarean delivery.
- Medical Procedures: Interventions such as dilation and curettage (D&C), hysteroscopy, or the insertion of intrauterine devices (IUDs) can introduce bacteria into the uterine cavity.
- Tuberculosis: In rare cases, Mycobacterium tuberculosis can infect the endometrium, leading to tuberculous endometritis.
Risk Factors
Several factors increase the likelihood of developing endometritis:
- Cesarean Delivery: Higher risk compared to vaginal births.
- Prolonged Labor: Extended duration increases exposure to potential pathogens.
- Multiple Vaginal Examinations: Frequent examinations during labor can introduce bacteria.
- Presence of STIs: Active infections elevate the risk.
- Use of IUDs: Particularly if inserted under non-sterile conditions.
Symptoms
The clinical presentation of endometritis may include:
- Fever: Often exceeding 38.3°C (101°F).
- Lower Abdominal or Pelvic Pain: Ranging from mild discomfort to severe pain.
- Abnormal Vaginal Bleeding or Discharge: May be purulent or have an unusual odor.
- Painful Urination or Bowel Movements: Due to pelvic inflammation.
- General Malaise: Including fatigue and a sense of discomfort.
Diagnosis
Accurate diagnosis involves:
- Pelvic Examination: Assessing for uterine tenderness and abnormal discharge.
- Laboratory Tests:
- Complete Blood Count (CBC): Elevated white blood cell count indicating infection.
- Cervical Cultures: Identifying specific pathogens like Chlamydia or Gonorrhea.
- Imaging Studies: Ultrasound may reveal retained products of conception or abscesses.
- Endometrial Biopsy: Particularly in chronic cases, to detect plasma cell infiltration indicative of chronic inflammation.
Treatment
Management strategies include:
- Antibiotic Therapy: Broad-spectrum antibiotics targeting the identified pathogens are the mainstay of treatment.
- Hospitalization: Required for severe cases, especially postpartum infections, to administer intravenous antibiotics and monitor the patient.
- Surgical Intervention: In instances of abscess formation or retained placental tissue, surgical procedures may be necessary to remove infected material.
Impact on Fertility
Untreated or chronic endometritis can lead to complications affecting fertility:
- Chronic Inflammation: May cause scarring and adhesions within the uterine cavity, known as Asherman’s syndrome.
- Impaired Embryo Implantation: Inflammatory changes can hinder the implantation process, leading to infertility or recurrent pregnancy loss.
Prevention
Preventative measures encompass:
- Safe Sexual Practices: Utilizing protection to reduce the risk of STIs.
- Aseptic Techniques: Ensuring sterile conditions during childbirth and medical procedures involving the uterus.
- Prophylactic Antibiotics: Administering antibiotics before cesarean sections or invasive gynecological procedures to minimize infection risk.

