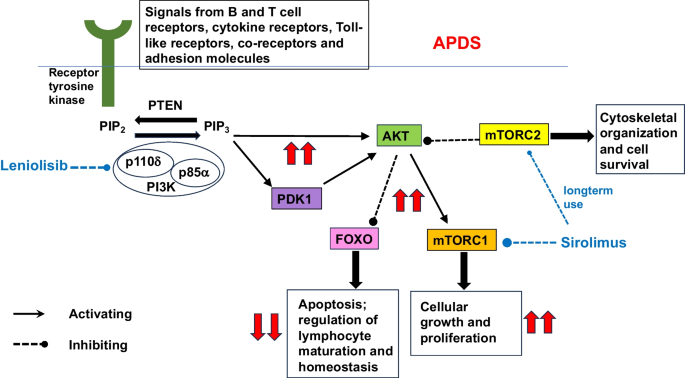
Activated Phosphoinositide 3-Kinase Delta Syndrome (APDS) is a rare primary immunodeficiency caused by genetic mutations in the PIK3CD or PIK3R1 genes, which regulate the phosphoinositide 3-kinase (PI3K) delta pathway. This condition disrupts immune cell function, leading to recurring infections, immune dysregulation, and other complications. Understanding the genetic basis, clinical manifestations, diagnostic procedures, and treatment options is essential for improving patient outcomes.
What Is Activated Phosphoinositide 3-Kinase Delta Syndrome?
APDS is a monogenic disorder that affects the PI3K delta pathway, crucial for the proper functioning of B cells, T cells, and natural killer (NK) cells. Mutations in the PIK3CD or PIK3R1 genes result in hyperactivation of this pathway, causing immune system abnormalities such as impaired antibody responses, susceptibility to infections, and inflammatory diseases.
Key Features of APDS
- Recurring Infections: Patients often experience chronic respiratory tract infections, which may lead to bronchiectasis if left untreated.
- Autoimmune Disorders: APDS can result in conditions such as autoimmune cytopenias, arthritis, or inflammatory bowel disease.
- Lymphoproliferation: Enlargement of lymph nodes, spleen, and other lymphoid tissues is a hallmark of APDS.
- Developmental Delays: In some cases, neurodevelopmental issues or growth delays may occur.
Genetic Basis and Pathophysiology
The PI3K delta pathway plays a critical role in the immune system by regulating cell survival, growth, and signaling. Mutations in the genes associated with APDS lead to uncontrolled PI3K signaling, disrupting immune cell function and homeostasis.
Genetic Mutations
- PIK3CD Mutations: Gain-of-function mutations in the PIK3CD gene result in excessive PI3K delta activation, affecting T and B cell development and function.
- PIK3R1 Mutations: Mutations in this gene, which encodes a regulatory subunit of PI3K delta, disrupt normal PI3K signaling and immune responses.
Mechanism of Immune Dysfunction
Excessive activation of the PI3K delta pathway alters cytokine production, reduces immune cell proliferation, and impairs the generation of effective immune responses. This mechanism underpins the susceptibility to infections and other complications in APDS patients.
Clinical Manifestations of APDS
The clinical presentation of APDS varies among patients but typically includes the following:
- Frequent Respiratory Infections: Sinusitis, otitis media, and pneumonia are common.
- Lymphoproliferation: Persistent enlargement of lymph nodes, spleen, and tonsils.
- Autoimmunity: Hemolytic anemia, immune thrombocytopenia, or other autoimmune conditions.
- Gastrointestinal Issues: Chronic diarrhea, malabsorption, and inflammatory bowel disease.
- Other Symptoms: Fatigue, failure to thrive, and developmental delays.
Diagnosis of Activated Phosphoinositide 3-Kinase Delta Syndrome
Timely diagnosis of APDS is essential for initiating appropriate treatments. Diagnosis involves a combination of clinical assessment, laboratory tests, and genetic analysis.
Diagnostic Steps
- Clinical History and Examination: Recurring infections, lymphoproliferation, and autoimmune features raise suspicion of APDS.
- Immunologic Testing:
- Reduced levels of immunoglobulins or specific antibody deficiencies.
- Impaired T cell responses.
- Genetic Testing: Sequencing of the PIK3CD and PIK3R1 genes confirms the diagnosis.
- Functional Assays: Evaluation of PI3K delta pathway activity to support genetic findings.
Treatment and Management of APDS
Management of APDS aims to control symptoms, prevent complications, and address underlying immune dysregulation.
Pharmacologic Treatments
- PI3K Delta Inhibitors: Targeted therapies such as leniolisib specifically inhibit the hyperactive PI3K delta pathway, improving immune function.
- Immunoglobulin Replacement Therapy (IRT): Regular IRT provides passive immunity and reduces infection rates.
- Antimicrobials: Prophylactic antibiotics or antivirals may be necessary to prevent infections.
Advanced Therapeutic Approaches
- Hematopoietic Stem Cell Transplantation (HSCT): The only curative option, HSCT replaces defective immune cells with healthy donor cells.
- Gene Therapy: Emerging experimental approaches focus on correcting the genetic mutations causing APDS.
Supportive Care
- Monitoring and Prevention: Regular follow-ups and monitoring of pulmonary function and infection status.
- Nutritional Support: Addressing malnutrition or deficiencies caused by chronic gastrointestinal issues.
While APDS remains a challenging condition, advances in targeted therapies and genetic interventions offer hope for better outcomes. Early diagnosis, personalized treatment plans, and ongoing research are key to managing the disease and improving quality of life for affected individuals.