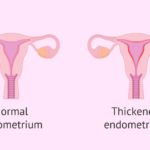
Endometrial carcinoma adjunct treatment, originating from the lining of the uterus, is one of the most prevalent gynecological malignancies. While early-stage diagnoses often lead to favorable outcomes with surgical interventions, the risk of recurrence persists, particularly in high-risk cases. Adjuvant treatments—therapies administered post-surgery—play a pivotal role in mitigating this risk and improving patient survival rates. This article explores various adjuvant treatment modalities for endometrial carcinoma, focusing on recent advancements and the integration of molecular classifications in therapeutic decision-making.

Molecular Classification and Its Impact on Treatment
Traditionally, endometrial carcinoma treatment has relied on histopathological evaluation. However, molecular classification has revolutionized this paradigm, offering a more precise understanding of tumor behavior and prognosis. The Cancer Genome Atlas (TCGA) has identified four distinct molecular subtypes of endometrial cancer:
- POLE-ultramutated: Characterized by mutations in the DNA polymerase epsilon gene, these tumors exhibit an exceptionally high mutation rate and are associated with a favorable prognosis.
- Microsatellite Instability-High (MSI-H): These tumors display defects in the mismatch repair system, leading to high microsatellite instability.
- Copy Number Low (CN-Low): Often referred to as the “no specific molecular profile” (NSMP), these tumors exhibit low copy number alterations.
- Copy Number High (CN-High): Also known as serous-like or p53-abnormal, these tumors are characterized by extensive copy number alterations and TP53 mutations, correlating with a poorer prognosis.
Integrating molecular classification into clinical practice enables a more personalized adjuvant treatment approach, optimizing therapeutic efficacy while minimizing unnecessary interventions.
Adjuvant Radiotherapy
Radiotherapy has long been a cornerstone in the adjuvant treatment of endometrial carcinoma, particularly for patients with high-intermediate and high-risk disease profiles. The primary modalities include:
External Beam Radiotherapy (EBRT)
EBRT involves directing radiation at the pelvic region to eradicate residual cancer cells post-surgery. While effective in reducing locoregional recurrence, EBRT is associated with significant acute and chronic toxicities. Studies indicate that EBRT does not significantly improve overall survival rates compared to other modalities.
Vaginal Brachytherapy (VBT)
VBT entails the placement of a radiation source within the vaginal vault, targeting potential residual disease with minimal exposure to surrounding tissues. Clinical trials have shown that VBT offers comparable efficacy to EBRT in preventing vaginal recurrences while maintaining a more favorable side effect profile. Consequently, VBT is often preferred, especially in patients with a lower risk of pelvic recurrence.
Adjuvant Chemotherapy
Chemotherapy serves as a systemic treatment modality, addressing potential micrometastatic disease. Its role is particularly emphasized in advanced-stage and high-risk endometrial carcinoma.
Chemotherapy Regimens
The combination of carboplatin and paclitaxel has emerged as a standard regimen, balancing efficacy and tolerability. This combination has demonstrated improved progression-free survival rates in high-risk patients.
Integration with Radiotherapy
The synergistic potential of combining chemotherapy with radiotherapy has been explored to enhance therapeutic outcomes. Notable studies include:
- PORTEC-3 Trial: This trial evaluated the addition of concurrent and adjuvant chemotherapy to EBRT in high-risk endometrial cancer patients. Results indicated an improvement in failure-free survival with the combined modality, particularly in stage III and serous cancers.
- GOG-258 Trial: This study compared chemoradiotherapy versus chemotherapy alone in advanced endometrial carcinoma. Findings revealed that while chemoradiotherapy reduced locoregional recurrences, it did not significantly impact overall survival compared to chemotherapy alone.
These studies underscore the importance of individualized treatment planning, considering factors such as stage, histology, and molecular subtype.
Immunotherapy and Targeted Therapies
Advancements in understanding the molecular underpinnings of endometrial carcinoma have paved the way for targeted therapies and immunotherapeutic approaches.
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors have shown promise, particularly in tumors with specific molecular alterations:
- Pembrolizumab: Approved for use in advanced endometrial cancers with high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR), pembrolizumab has demonstrated durable responses in this subset of patients.
- Dostarlimab: This PD-1 inhibitor has received approval for treating recurrent or advanced dMMR endometrial cancer, offering a new avenue for patients with limited treatment options.
Molecularly Targeted Therapies
Research into targeted therapies continues to evolve:
- mTOR Inhibitors: Agents targeting the mTOR pathway have shown potential in treating recurrent endometrial cancer, particularly in cases resistant to conventional therapies.
- PARP Inhibitors: For tumors harboring specific DNA repair deficiencies, PARP inhibitors have emerged as a promising therapeutic option.
Future Directions and Conclusion
With ongoing advancements in molecular profiling, the treatment landscape for endometrial carcinoma continues to evolve. The integration of molecular classification has refined treatment strategies, enabling personalized approaches that optimize outcomes while reducing unnecessary toxicity. The combination of chemotherapy, radiotherapy, immunotherapy, and targeted therapies holds promise for improving patient survival rates.
Future research should focus on refining these therapeutic strategies, identifying novel biomarkers, and developing combination regimens to further enhance treatment efficacy. As precision medicine advances, individualized adjuvant treatments will play an increasingly central role in managing endometrial carcinoma, ultimately improving patient prognoses.