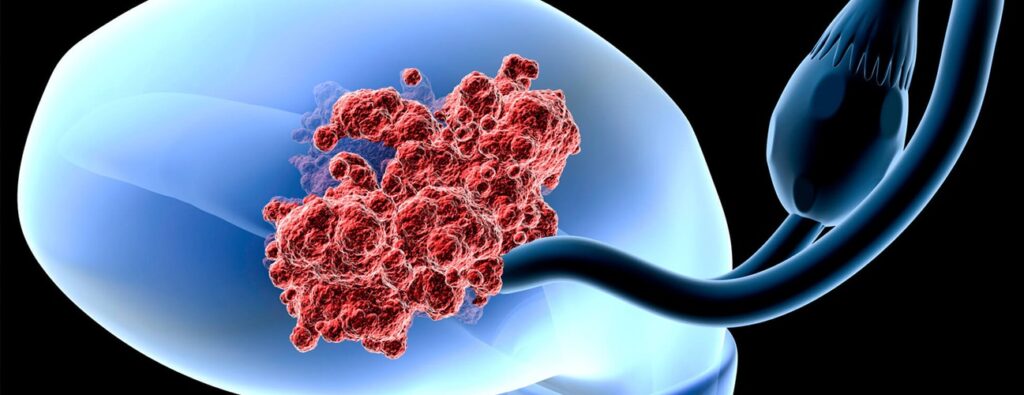
Endometrial carcinoma is the most common gynecologic malignancy in developed countries. Originating in the inner lining of the uterus (endometrium), this cancer primarily affects postmenopausal women. The increasing incidence underscores the need for awareness, early detection, and effective treatment.
Pathophysiology of Endometrial Carcinoma
Endometrial carcinoma develops when genetic mutations trigger uncontrolled cell growth in the endometrium. This can result from hormonal imbalances, genetic predispositions, or environmental factors.
Types of Endometrial Carcinoma
Endometrial carcinoma is classified into two major types:
- Type I (Estrogen-Dependent)
- Includes endometrioid adenocarcinoma (most common).
- Typically low-grade, slow-growing, and associated with excess estrogen.
- Often linked to obesity, polycystic ovary syndrome (PCOS), and hormone replacement therapy.
- Type II (Non-Estrogen-Dependent)
- Includes serous carcinoma, clear cell carcinoma, and other rare subtypes.
- More aggressive, with a poorer prognosis.
- Not strongly linked to hormonal imbalance.
Risk Factors
Several factors increase the likelihood of developing endometrial carcinoma:
- Hormonal Factors: Unopposed estrogen exposure due to obesity, anovulation, or hormone therapy.
- Age: Most cases occur in postmenopausal women.
- Genetic Syndromes: Lynch syndrome significantly elevates risk.
- Reproductive History: Nulliparity and late menopause increase susceptibility.
- Diabetes & Obesity: Excess adipose tissue raises estrogen levels.
- Tamoxifen Use: A breast cancer treatment that slightly increases endometrial cancer risk.
Clinical Presentation
The most common symptom of endometrial carcinoma is abnormal uterine bleeding. Additional signs include:
- Postmenopausal bleeding (most significant indicator).
- Heavy or irregular menstrual bleeding in premenopausal women.
- Pelvic pain or pressure.
- Watery or blood-tinged vaginal discharge.
- Pain during intercourse.
Diagnosis
Timely diagnosis improves outcomes. The diagnostic process includes:
- Pelvic Examination: Initial clinical assessment.
- Transvaginal Ultrasound (TVUS): Measures endometrial thickness.
- Endometrial Biopsy: Gold standard for diagnosis.
- Hysteroscopy with Biopsy: Direct visualization and targeted tissue sampling.
- Imaging: MRI and CT scans assess disease spread.
Staging
Endometrial carcinoma staging follows the FIGO system:
- Stage I: Confined to the uterus.
- Stage II: Invades cervical stroma but remains within the uterus.
- Stage III: Extends to nearby lymph nodes or structures.
- Stage IV: Spreads to distant organs like the bladder, bowel, or lungs.
Treatment Strategies
1. Surgery (Primary Treatment)
- Total Hysterectomy with Bilateral Salpingo-Oophorectomy (TH/BSO): Removal of the uterus, fallopian tubes, and ovaries.
- Lymph Node Dissection: Determines disease spread.
2. Radiation Therapy
- External Beam Radiation (EBRT): Used post-surgery to reduce recurrence risk.
- Brachytherapy: Internal radiation targeting residual cancer cells.
3. Chemotherapy
- Typically used in advanced or aggressive cases.
- Common agents: Carboplatin and Paclitaxel.
4. Hormonal Therapy
- Used for hormone-sensitive tumors.
- Medications: Progestins, Aromatase Inhibitors, Tamoxifen.
5. Targeted Therapy & Immunotherapy
- Dostarlimab (Immune Checkpoint Inhibitor): Effective in cases with specific genetic mutations.
- mTOR Inhibitors & Anti-VEGF Therapy: Target cancer cell growth pathways.
Prognosis & Survival Rates
- Stage I: 5-year survival rate >90%.
- Stage II: 5-year survival rate ~80%.
- Stage III: 5-year survival rate ~50%.
- Stage IV: 5-year survival rate ~15-20%.
Early-stage detection significantly improves survival outcomes.
Prevention & Risk Reduction
1. Weight Management & Exercise
Maintaining a healthy BMI reduces estrogen-related risk.
2. Birth Control Use
Long-term use of combined oral contraceptives lowers endometrial cancer risk.
3. Screening for High-Risk Individuals
- Women with Lynch syndrome should undergo regular endometrial sampling.
- Genetic counseling is recommended for individuals with a strong family history.
4. Early Symptom Awareness
Educating women about postmenopausal bleeding as a red flag for endometrial cancer.

