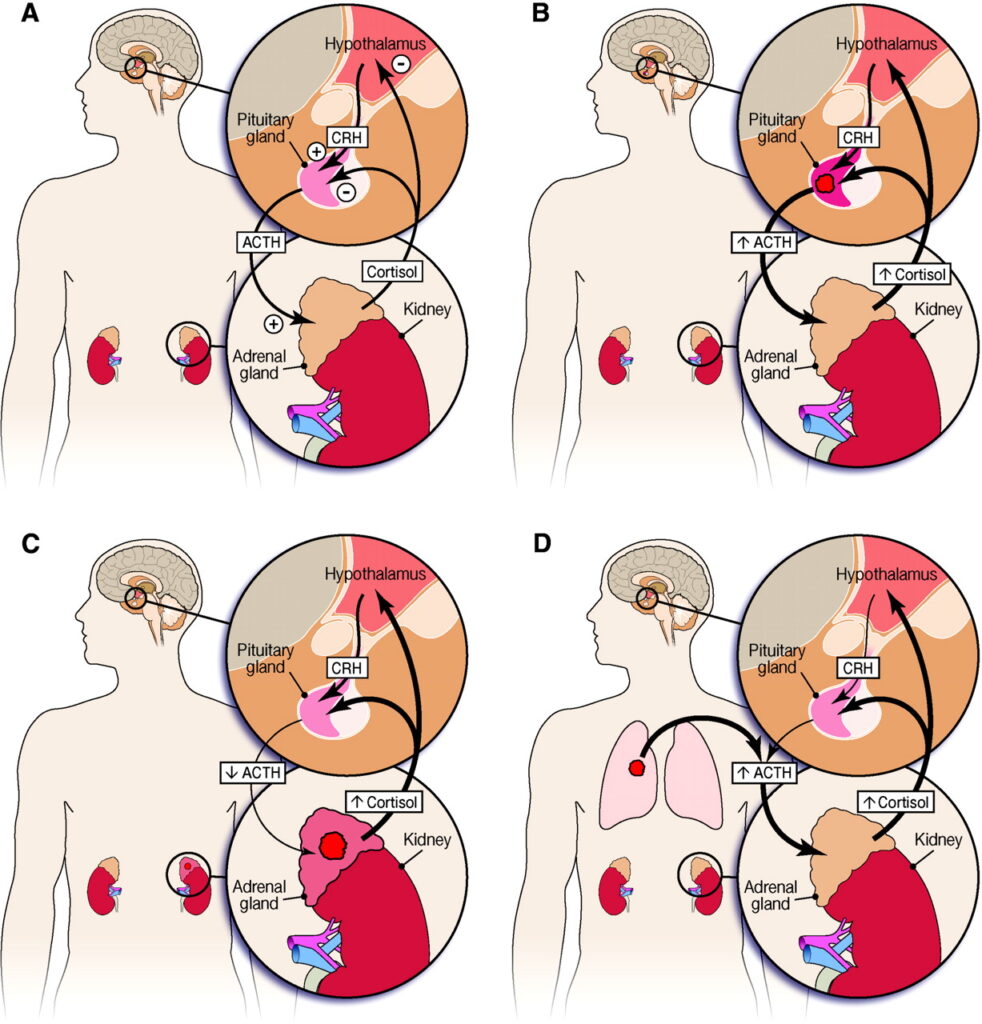
Ectopic Adrenocorticotropic Hormone (ACTH) Syndrome is a rare endocrine disorder characterized by the production of ACTH by non-pituitary tumors, leading to hypercortisolism and the clinical manifestations of Cushing’s syndrome. This condition poses significant diagnostic and therapeutic challenges due to its diverse etiology and presentation.
Pathophysiology of Ectopic ACTH Syndrome
Under normal physiological conditions, the hypothalamus secretes corticotropin-releasing hormone (CRH), which stimulates the anterior pituitary gland to release ACTH. ACTH then acts on the adrenal cortex to produce cortisol, a glucocorticoid hormone essential for various metabolic functions. In Ectopic ACTH Syndrome, non-pituitary tumors aberrantly produce ACTH, bypassing the regulatory feedback mechanisms and resulting in excessive cortisol production. This unregulated cortisol secretion leads to the clinical features associated with Cushing’s syndrome.
Etiology: Tumors Associated with Ectopic ACTH Production
A variety of neoplasms have been implicated in the ectopic production of ACTH. These tumors often originate from neuroendocrine cells and can be benign or malignant. Common tumors include:
- Pulmonary Tumors: Small cell lung carcinoma and bronchial carcinoids are the most frequent sources.
- Thymic Tumors: Thymic carcinoids, though less common, have been reported.
- Pancreatic Tumors: Islet cell tumors can occasionally produce ACTH.
- Medullary Thyroid Carcinoma: This thyroid malignancy has been associated with ectopic ACTH secretion.
The prevalence of these tumors varies, with pulmonary sources being the most common. The clinical presentation can differ based on the tumor’s location, size, and malignancy potential.
Clinical Manifestations
The excessive cortisol production in Ectopic ACTH Syndrome leads to a spectrum of clinical features, some of which may include:
- Metabolic Disturbances: Hyperglycemia, dyslipidemia, and weight gain.
- Cardiovascular Complications: Hypertension and increased risk of thromboembolic events.
- Musculoskeletal Issues: Proximal muscle weakness and osteoporosis.
- Dermatological Signs: Thin skin, easy bruising, and purple striae.
- Neuropsychiatric Symptoms: Depression, anxiety, and cognitive impairments.
The rapidity and severity of symptom onset can vary, often correlating with the tumor’s aggressiveness.
Diagnostic Approach
Diagnosing Ectopic ACTH Syndrome requires a systematic approach:
- Biochemical Confirmation: Elevated serum cortisol and ACTH levels, with a lack of suppression on dexamethasone suppression testing, suggest an ACTH-dependent Cushing’s syndrome.
- Localization of the Source: Imaging studies, including CT and MRI scans of the chest and abdomen, are employed to identify potential tumors. Functional imaging, such as somatostatin receptor scintigraphy or PET scans, may aid in detecting occult neoplasms.
- Inferior Petrosal Sinus Sampling (IPSS): This invasive procedure measures ACTH levels in the venous drainage of the pituitary gland compared to peripheral blood. A central-to-peripheral ACTH gradient indicates a pituitary source, whereas the absence of such a gradient suggests ectopic production. IPSS is particularly useful when imaging studies are inconclusive.
Treatment Modalities
Management strategies focus on both controlling hypercortisolism and addressing the underlying tumor:
- Surgical Resection: The definitive treatment involves the removal of the ACTH-secreting tumor. Surgical success depends on the tumor’s location and resectability.
- Medical Therapy: In cases where surgery is not feasible, medications such as ketoconazole, metyrapone, or mitotane can be used to inhibit cortisol synthesis.
- Radiation Therapy: Applicable for certain tumor types, especially when surgical options are limited.
- Bilateral Adrenalectomy: Considered a last resort, this procedure removes both adrenal glands to control cortisol levels but necessitates lifelong hormone replacement therapy.
Prognosis
The prognosis of Ectopic ACTH Syndrome varies based on several factors:
- Tumor Type and Malignancy: Benign tumors have a more favorable outcome compared to aggressive malignancies.
- Timeliness of Diagnosis and Treatment: Early identification and management of the underlying tumor can improve clinical outcomes.
- Control of Hypercortisolism: Effective management of cortisol levels is crucial in reducing morbidity and mortality associated with the syndrome.
Regular follow-up is essential to monitor for tumor recurrence and manage any long-term sequelae of hypercortisolism.