Actinomycosis is a rare but serious bacterial infection that primarily affects soft tissues, often leading to the formation of abscesses and tissue fibrosis. This guide provides an in-depth analysis of actinomycosis, its causes, symptoms, diagnosis, and treatment options, offering a complete resource for understanding and managing this condition effectively.
What is Actinomycosis?
Actinomycosis is a chronic bacterial infection caused by Actinomyces species, which are anaerobic or microaerophilic bacteria commonly found in the oral cavity, gastrointestinal tract, and female genital tract. These bacteria are generally harmless but can cause infection when tissue integrity is compromised.
Common Types of Actinomycosis
Actinomycosis can manifest in various forms depending on the site of infection. The most common types include:
- Cervicofacial Actinomycosis: Often referred to as “lumpy jaw,” this type typically occurs after dental trauma or infection.
- Thoracic Actinomycosis: Affects the lungs, chest wall, or other thoracic structures.
- Abdominal Actinomycosis: Results from gastrointestinal perforations or surgeries.
- Pelvic Actinomycosis: Commonly associated with intrauterine devices (IUDs).
- Cutaneous Actinomycosis: Involves the skin, usually due to direct trauma.
Causes and Risk Factors
Actinomycosis is caused when Actinomyces bacteria breach the mucosal barrier and invade deeper tissues. Several factors can contribute to this:
- Dental Infections: Poor oral hygiene or invasive dental procedures.
- Trauma or Surgery: Injuries or surgeries that expose deep tissues.
- Gastrointestinal Conditions: Conditions like diverticulitis or appendicitis.
- Prolonged IUD Use: Pelvic actinomycosis often arises due to long-term use of intrauterine devices.
- Immunosuppression: Weakened immune systems increase susceptibility to infection.
Symptoms of Actinomycosis
The clinical presentation of actinomycosis varies based on the site of infection. Common symptoms include:
- Swelling or masses with a woody consistency.
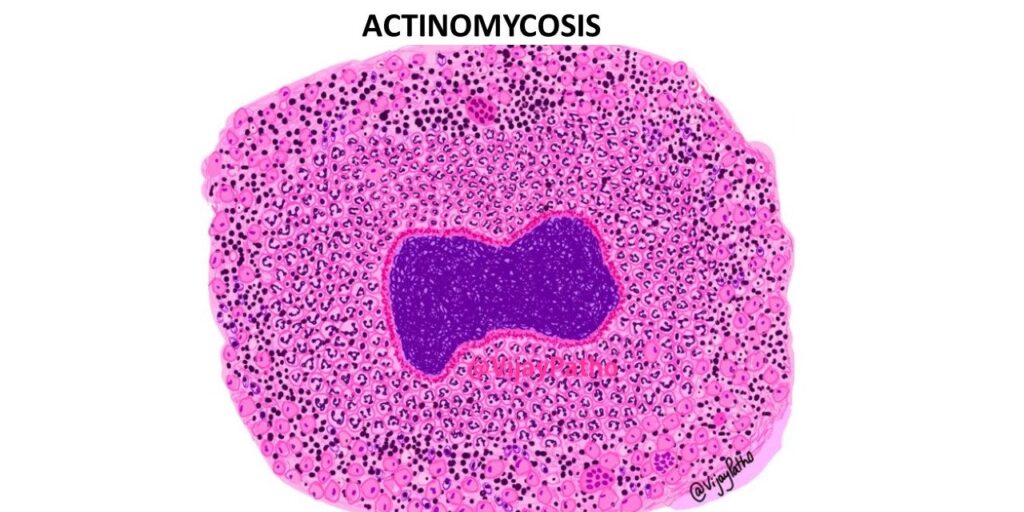
- Draining sinus tracts exuding pus, often with yellow sulfur granules.
- Fever, fatigue, and weight loss.
- Pain localized to the affected area.
- Difficulty swallowing (cervicofacial actinomycosis).
- Respiratory symptoms such as cough and chest pain (thoracic actinomycosis).
- Abdominal pain and bloating (abdominal actinomycosis).
Diagnosing Actinomycosis
Diagnosing actinomycosis requires a combination of clinical evaluation, imaging, and microbiological studies. Steps include:
- Patient History: Assessing risk factors like recent dental work, surgeries, or IUD use.
- Physical Examination: Identifying characteristic symptoms such as masses or sinus tracts.
- Imaging Studies:
- CT scans or MRIs reveal tissue involvement and abscess formation.
- X-rays may help identify thoracic lesions.
- Microbiological Testing:
- Pus or tissue biopsy is analyzed for Actinomyces bacteria.
- Culture growth confirms the diagnosis but may take up to two weeks.
Treatment and Management of Actinomycosis
Successful treatment of actinomycosis involves prolonged antibiotic therapy, often combined with surgical interventions to remove infected tissue.
Antibiotic Therapy
- Primary Antibiotics:
- High-dose Penicillin G is the first-line treatment, administered intravenously for 2–6 weeks.
- Oral antibiotics like amoxicillin or doxycycline are continued for 6–12 months.
- Alternative Antibiotics:
- Clindamycin or erythromycin for penicillin-allergic patients.
Surgical Intervention
In cases with extensive abscesses or tissue damage, surgical drainage or excision may be required to complement antibiotic therapy.
Prevention Strategies
While actinomycosis is rare, preventive measures can reduce risk:
- Maintain good oral hygiene and seek timely dental care.
- Manage gastrointestinal conditions promptly to avoid perforations.
- Replace IUDs as recommended by healthcare providers.
- Strengthen the immune system through a balanced diet and regular health check-ups.
Actinomycosis, though rare, can lead to severe complications if untreated. Early diagnosis and prompt treatment with antibiotics and, where necessary, surgical intervention are critical for favorable outcomes. By understanding the risk factors and symptoms, patients and healthcare providers can work together to manage and prevent this condition effectively.

