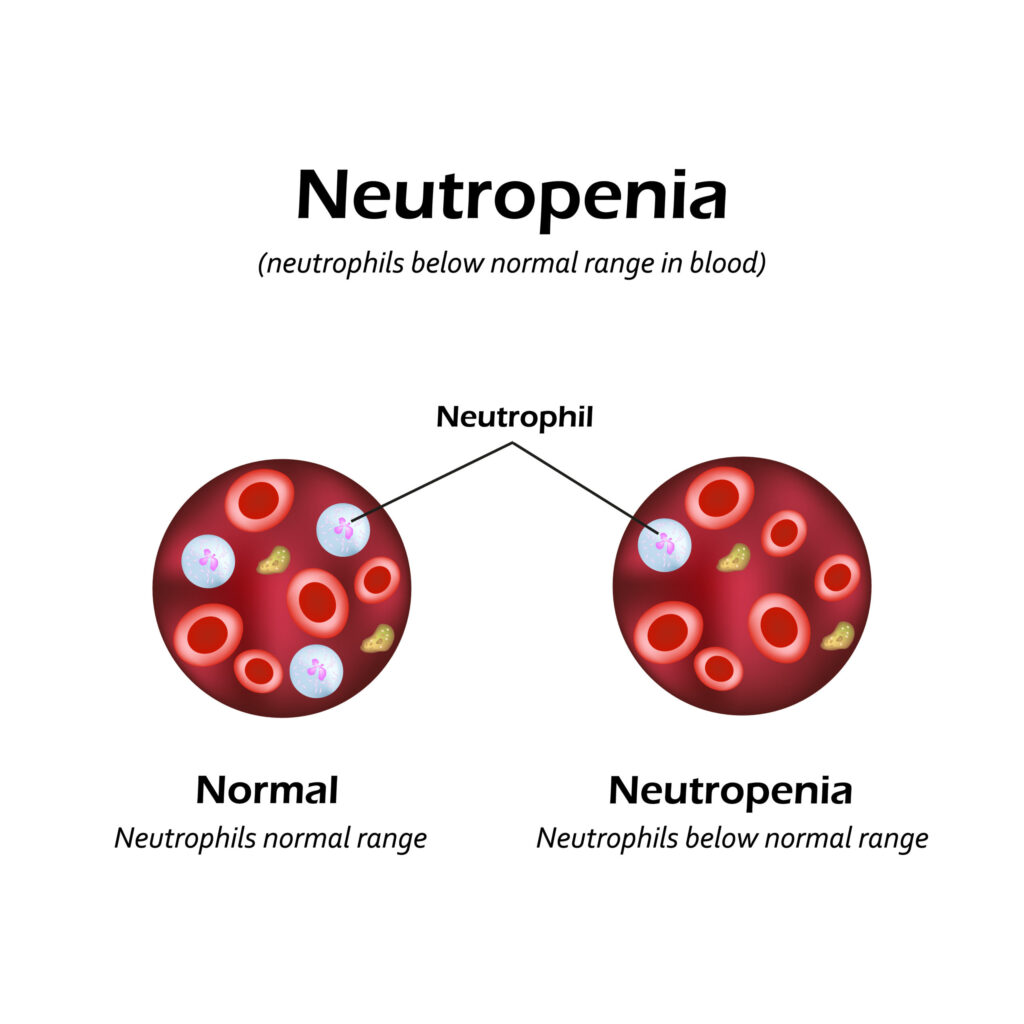
Drug-induced neutropenia is a hematologic disorder characterized by an abnormally low neutrophil count, increasing susceptibility to infections. This condition arises as an adverse reaction to various medications, ranging from chemotherapy agents to non-chemotherapy drugs such as antibiotics, antipsychotics, and antithyroid medications. Given the potential severity of this condition, early detection and intervention are crucial for preventing life-threatening complications.
Mechanisms of Drug-Induced Neutropenia
The development of drug-induced neutropenia occurs through two primary mechanisms:
Decreased Neutrophil Production
Some drugs exert direct toxicity on bone marrow progenitor cells, impairing their ability to produce neutrophils. This suppression can occur due to inhibition of myeloid cell differentiation, cytotoxic effects on stem cells, or disruption of hematopoietic growth factors. Medications such as antithyroid drugs and chemotherapy agents are known to interfere with neutrophil production.
Increased Neutrophil Destruction
Certain medications trigger immune-mediated destruction of neutrophils. This process occurs when drug-related metabolites act as haptens, forming neoantigens that stimulate the immune system to produce anti-neutrophil antibodies. The result is accelerated clearance of neutrophils, leading to profound neutropenia.
High-Risk Medications
Several drug classes have been implicated in drug-induced neutropenia, with varying degrees of risk:
Antithyroid Drugs
- Propylthiouracil
- Methimazole
These drugs are commonly associated with bone marrow suppression, necessitating regular monitoring of blood counts.
Antipsychotics
- Clozapine
Clozapine-induced agranulocytosis is a well-documented adverse reaction, requiring strict hematologic monitoring.
Antibiotics
- Beta-lactams (e.g., penicillins, cephalosporins)
- Sulfonamides
Certain antibiotics can trigger neutropenia via immune-mediated destruction or direct marrow suppression.
Antiplatelet Agents
- Ticlopidine
This medication, once widely used, has been largely replaced by alternatives with better safety profiles due to its risk of severe neutropenia.
Clinical Manifestations
The severity of symptoms depends on the depth and duration of neutropenia:
Early Symptoms
- Fever
- Chills
- Sore throat
- Malaise
These nonspecific symptoms often precede more serious complications.
Severe Infections
- Pneumonia
- Septicemia
- Mucosal ulcers
- Sepsis and septic shock
Profound neutropenia impairs immune function, increasing the risk of life-threatening infections.
Diagnostic Approaches
Laboratory Investigations
- Complete Blood Count (CBC): Confirms neutropenia.
- Absolute Neutrophil Count (ANC): <1.5 × 10⁹/L indicates neutropenia; <0.5 × 10⁹/L is considered severe.
- Peripheral Blood Smear: May reveal neutropenia with normal red blood cell and platelet counts.
Bone Marrow Examination
- Conducted in cases of persistent or unexplained neutropenia to assess bone marrow function.
Management Strategies
Discontinuation of the Causative Drug
- Immediate cessation often leads to gradual recovery of neutrophil levels.
Infection Management
- Empirical Broad-Spectrum Antibiotics: Initiated in febrile neutropenic patients.
- Antifungal Therapy: Considered if fever persists despite antibiotics.
Hematopoietic Growth Factors
- Granulocyte Colony-Stimulating Factor (G-CSF): Accelerates neutrophil recovery and reduces infection risks.
Supportive Care
- Isolation Precautions: Reduces exposure to infectious agents.
- Frequent Monitoring: Regular CBC assessments guide treatment decisions.

