Disseminated neonatal herpes simplex infection is a severe viral condition affecting newborns, primarily caused by the herpes simplex virus (HSV). It represents a significant challenge in neonatal care due to its potential for causing life-threatening complications. This article provides an in-depth understanding of disseminated neonatal herpes, its causes, clinical presentation, diagnostic methods, treatment strategies, and preventive measures.

What is Disseminated Neonatal Herpes Simplex Infection?
Disseminated neonatal herpes simplex infection refers to a widespread infection in a newborn caused by the herpes simplex virus. This condition can involve multiple organs, including the skin, eyes, liver, lungs, and brain, and is considered the most severe form of neonatal herpes. It occurs when the virus spreads throughout the body, leading to systemic symptoms and potentially fatal outcomes without prompt treatment.
There are two main types of herpes simplex virus:
- HSV-1: Commonly associated with oral herpes, though it can also cause neonatal herpes.
- HSV-2: Typically linked to genital herpes, this strain is more frequently responsible for neonatal infections.
Key Causes of Disseminated Neonatal Herpes Simplex Infection
The primary mode of transmission of HSV to neonates is through vertical transmission, where the virus is passed from mother to child during childbirth. The following are the main factors contributing to neonatal HSV infection:
- Maternal Active HSV Infection: If a mother has an active genital HSV infection at the time of delivery, the baby is at a high risk of contracting the virus.
- Asymptomatic Viral Shedding: Even without visible symptoms, the virus can still be shed by an infected mother, leading to transmission.
- Primary Infection vs. Recurrent Infection: Newborns are more likely to develop severe infection if the mother experiences a primary HSV infection during pregnancy, rather than a recurrent one, as the infant has no pre-existing immunity.
Symptoms of Disseminated Neonatal Herpes Simplex Infection
The symptoms of neonatal herpes can vary widely depending on the severity and the organs involved. In cases of disseminated infection, the following clinical signs may present:
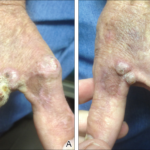
- Skin Lesions: Vesicular skin lesions, often in a cluster, are common in neonatal HSV infections. These lesions are typically located on the face, trunk, or limbs.
- Neurological Symptoms: Seizures, lethargy, poor feeding, and irritability may indicate involvement of the central nervous system.
- Respiratory Distress: Difficulty breathing, rapid breathing, or cyanosis can occur when the lungs are involved.
- Gastrointestinal and Liver Dysfunction: Jaundice, hepatomegaly, and abnormal liver function tests may occur if the liver is affected.
- Eye Involvement: Conjunctivitis, keratitis, or retinitis can occur, leading to vision problems or blindness if untreated.
Stages of Neonatal Herpes Infection
Neonatal herpes simplex infection can present in three distinct clinical stages:
- Localized Skin, Eye, and Mouth (SEM) Disease: This is the mildest form, where the infection is confined to the skin and mucous membranes.
- Central Nervous System (CNS) Disease: Involvement of the brain, leading to encephalitis, seizures, or abnormal neurologic development.
- Disseminated Disease: This severe form involves multiple organs and is life-threatening without immediate intervention.
Diagnosis of Disseminated Neonatal Herpes Simplex Infection
Accurate and early diagnosis is crucial for managing neonatal herpes. The following diagnostic approaches are commonly used:
- Polymerase Chain Reaction (PCR): PCR testing of skin lesions, blood, cerebrospinal fluid (CSF), or other bodily fluids is the gold standard for detecting HSV DNA.
- Virus Culture: Culture of the virus from lesion samples or CSF can help confirm the diagnosis but may be less sensitive than PCR.
- Serology: Blood tests to detect HSV antibodies can help identify past exposure but are not useful in diagnosing active infections in newborns.
- Clinical Evaluation: A thorough clinical evaluation, including the history of maternal HSV infection and the timing of birth, is essential for diagnosis.
Differentiating Neonatal Herpes from Other Neonatal Infections
Given the broad spectrum of symptoms associated with neonatal herpes, it is essential to differentiate it from other neonatal infections such as sepsis, bacterial meningitis, or viral encephalitis. This requires a combination of clinical signs, laboratory tests, and imaging studies.
Treatment of Disseminated Neonatal Herpes Simplex Infection
Prompt antiviral treatment is essential for improving outcomes in infants with disseminated neonatal herpes simplex infection. The treatment options include:
- Acyclovir: The primary treatment for neonatal herpes is intravenous acyclovir, which inhibits the replication of the herpes simplex virus. Treatment should start as soon as possible after diagnosis, ideally within 24 hours.
- Supportive Care: Infants with severe infections often require intensive care, including respiratory support, hydration, and management of organ dysfunction.
- Prognosis: The prognosis of disseminated neonatal herpes depends on the speed of diagnosis and treatment. Early intervention can significantly improve survival rates and reduce the risk of long-term neurological damage.
Long-Term Management and Follow-Up
Infants who survive disseminated neonatal herpes may require long-term follow-up to monitor for potential complications, particularly neurological deficits. Cognitive and developmental assessments, along with regular eye and hearing screenings, are essential parts of post-infection care.
Prevention of Neonatal Herpes Simplex Infection
Preventing neonatal herpes infection primarily focuses on reducing the risk of transmission from mother to child during labor and delivery:
- Antiviral Therapy for Mothers: Pregnant women with a history of HSV infection or recurrent outbreaks may be prescribed acyclovir or valacyclovir in the third trimester to reduce the risk of transmission during delivery.
- Cesarean Delivery: In cases where the mother has an active genital herpes infection at the time of delivery, a cesarean section is often recommended to reduce the risk of vertical transmission.
- Postnatal Prophylaxis: Newborns born to mothers with active herpes infections may receive antiviral treatment to prevent the onset of symptoms.
Maternal Screening and Counseling
Screening for HSV in pregnant women, particularly those with a history of genital herpes, can help identify at-risk pregnancies. Counseling regarding the risks of HSV transmission, the use of antivirals, and delivery options can aid in reducing the incidence of neonatal herpes.