Disseminated Intravascular Coagulation (DIC) is a serious medical condition characterized by widespread activation of the clotting cascade, leading to both clot formation and bleeding. This paradoxical situation occurs when clotting factors and platelets are consumed at a faster rate than they can be replenished, causing severe bleeding and thrombus formation throughout the body. Due to its complex and often critical nature, timely diagnosis and treatment of DIC are crucial for patient survival and recovery.

What is Disseminated Intravascular Coagulation (DIC)?
DIC is a systemic disorder in which the body’s natural clotting mechanisms are disrupted, leading to the formation of small blood clots in the bloodstream. These microthrombi can block the flow of blood to vital organs, causing damage. At the same time, the excessive clotting depletes platelets and coagulation proteins, leading to a heightened risk of bleeding.
While DIC is not a primary disease but rather a complication of other conditions, it presents a significant challenge for healthcare professionals due to its dual nature—simultaneous clotting and bleeding.
Causes of Disseminated Intravascular Coagulation
DIC can be triggered by a variety of underlying conditions, such as:
- Sepsis: Severe infections, particularly bacterial infections, are one of the most common triggers for DIC. Bacteria release toxins that can activate the clotting cascade.
- Trauma or Surgery: Major surgeries or traumatic injuries that cause extensive tissue damage can lead to DIC.
- Cancer: Certain types of cancer, including pancreatic, lung, and prostate cancers, can increase the risk of DIC.
- Obstetric Complications: Conditions like placental abruption, eclampsia, and retained dead fetus syndrome during pregnancy can trigger DIC.
- Severe Burns: Large-scale burns can result in tissue damage and the release of clotting factors.
- Liver Disease: The liver produces many coagulation factors, and liver dysfunction can cause an imbalance in clotting mechanisms.
- Snake Bites or Toxins: Certain venomous snake bites can trigger the clotting cascade, leading to DIC.
Symptoms of Disseminated Intravascular Coagulation
Symptoms of DIC are highly variable and depend on the severity and stage of the condition. Common symptoms include:
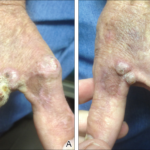
- Bleeding: Uncontrolled bleeding, such as from gums, nosebleeds, bruising, or internal bleeding, is a hallmark of DIC.
- Shortness of Breath: Blood clots in the lungs (pulmonary embolism) can result in respiratory distress.
- Drop in Blood Pressure: As a result of excessive bleeding and clot formation, the blood pressure may fall, leading to shock.
- Organ Dysfunction: Clots blocking blood flow can result in organ failure, particularly affecting the kidneys, liver, and brain.
- Purpura: The appearance of purple or red skin spots due to small vessel hemorrhages.
- Elevated D-Dimer Levels: D-dimer is a breakdown product of fibrin, and its elevated levels are often a marker of DIC.
Diagnosis of Disseminated Intravascular Coagulation
Diagnosing DIC requires a thorough clinical assessment, including a review of the patient’s medical history and risk factors. Common diagnostic tests for DIC include:
- Complete Blood Count (CBC): Low platelet counts may indicate DIC.
- Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT): These tests measure how long it takes for blood to clot and may be prolonged in DIC.
- Fibrinogen Levels: Decreased fibrinogen levels are indicative of DIC, as fibrinogen is consumed during clot formation.
- D-Dimer Test: Elevated D-dimer levels indicate the presence of fibrin degradation, a key feature of DIC.
- Peripheral Smear: A blood smear may reveal fragmented red blood cells, a sign of microvascular thrombosis.
- Organ Function Tests: Given the potential for organ failure, kidney and liver function tests may be performed.
Early recognition is essential, as delayed diagnosis of DIC can result in irreversible organ damage and high mortality rates.
Treatment and Management of Disseminated Intravascular Coagulation
The treatment of DIC revolves around managing the underlying condition, supporting organ function, and controlling both clotting and bleeding. The approach may include:
- Addressing the Underlying Cause: The most important step in managing DIC is treating the condition that triggered it. This could involve administering antibiotics for infections, surgical intervention for trauma, or chemotherapy for cancers.
- Platelet and Coagulation Factor Replacement: Blood products, such as platelets, fresh frozen plasma, and cryoprecipitate, may be administered to replace depleted clotting factors.
- Anticoagulation Therapy: In some cases, anticoagulants such as heparin may be used to prevent further clot formation, though its use is controversial and should be carefully considered.
- Supportive Care: Patients with severe bleeding may require blood transfusions or vasopressor medications to support blood pressure and organ perfusion.
- Organ Support: Dialysis may be necessary for kidney failure, while mechanical ventilation may be required for respiratory failure.
Prognosis of Disseminated Intravascular Coagulation
The prognosis for patients with DIC depends largely on the severity of the condition, the underlying cause, and how quickly treatment is initiated. In general, the earlier DIC is diagnosed and treated, the better the chances of recovery. If DIC is left untreated, it can result in multi-organ failure, significant bleeding, and death.
Outcomes are better for patients who recover from the underlying cause of DIC, but those with severe complications such as renal failure or hemorrhagic shock may have a poor prognosis.
Prevention of Disseminated Intravascular Coagulation
Although DIC cannot always be prevented, certain measures can reduce the risk, particularly in individuals at high risk:
- Infection Control: Proper hygiene, vaccination, and early treatment of infections, especially sepsis, are important in preventing DIC.
- Timely Management of Pregnancy Complications: Close monitoring of pregnant women for conditions like preeclampsia and placental abruption can prevent the onset of DIC.
- Trauma and Surgery Care: Proper management of trauma and post-surgical care is essential to prevent DIC, especially in high-risk surgeries.
- Cancer Surveillance: Early detection and treatment of cancers can reduce the risk of DIC in at-risk patients.