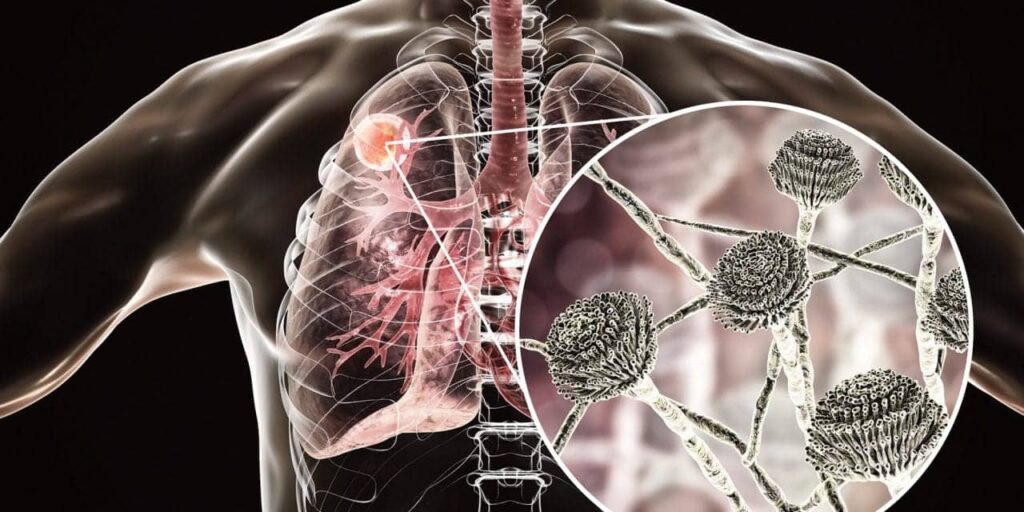
Disseminated coccidioidomycosis is a severe, systemic fungal infection caused by Coccidioides species, primarily Coccidioides immitis and Coccidioides posadasii. Endemic to arid regions of the southwestern United States, parts of Mexico, Central, and South America, this condition arises when the infection extends beyond the pulmonary system to other body parts, including skin, bones, joints, and the central nervous system. Understanding its etiology, clinical manifestations, diagnostic approaches, and treatment options is crucial for effective management.
Etiology and Epidemiology
Coccidioides fungi thrive in alkaline, sandy soils of semiarid regions with hot summers and mild winters. The primary endemic areas include southern Arizona, central California, southwestern New Mexico, and west Texas. Infection occurs through inhalation of airborne arthroconidia (spores) released from disturbed soil. While many infections are asymptomatic or self-limiting, certain individuals are at increased risk for dissemination.
Risk Factors for Dissemination
Disseminated coccidioidomycosis occurs in approximately 1–3% of infected individuals. Risk factors include:
- Immunosuppression: Individuals with HIV/AIDS, organ transplant recipients, or those on immunosuppressive therapies.
- Ethnicity: Higher incidence observed in African American and Filipino populations.
- Pregnancy: Particularly during the third trimester and postpartum period.
- Underlying Health Conditions: Diabetes mellitus, chronic pulmonary diseases, and advanced age.
Clinical Manifestations
The clinical presentation varies based on the organs involved:
- Cutaneous Involvement: Skin manifestations occur in 15–20% of disseminated cases, presenting as ulcers, nodules, or erythema nodosum.
- Osteoarticular Involvement: Bone and joint infections can lead to osteomyelitis, causing localized pain and swelling.
- Central Nervous System: Meningitis is a severe complication, presenting with headaches, neck stiffness, photophobia, and altered mental status.
Diagnostic Approaches
Accurate diagnosis involves a combination of clinical evaluation, imaging, and laboratory testing:
- Serological Tests: Detection of specific IgM and IgG antibodies against Coccidioides spp.
- Culture and Microscopy: Isolation of the organism from clinical specimens and identification of characteristic spherules in tissues.
- Molecular Methods: Polymerase chain reaction (PCR) assays for rapid and specific detection.
Treatment Modalities
Management depends on the severity and extent of dissemination:
- Antifungal Therapy: First-line treatments include azole antifungals such as fluconazole or itraconazole. In severe cases, amphotericin B may be administered. Duration of therapy varies, often extending for several months to prevent relapse.
- Surgical Intervention: Indicated for drainage of abscesses or debridement of necrotic tissue in refractory cases.
Prevention Strategies
Preventive measures focus on reducing exposure, especially for high-risk individuals:
- Environmental Controls: Minimizing activities that disturb soil in endemic areas, such as construction or farming, to reduce airborne spores.
- Personal Protective Equipment: Use of N95 respirators for those in high-exposure occupations.
- Public Awareness: Educating at-risk populations about the signs and symptoms to facilitate early diagnosis and treatment.