Disseminated candidiasis represents a severe systemic infection caused by Candida species, notably Candida albicans. This condition arises when the fungus enters the bloodstream, leading to widespread organ involvement. It predominantly affects immunocompromised individuals, including those undergoing chemotherapy, organ transplantation, or prolonged intensive care unit (ICU) stays.
Etiology and Risk Factors
The primary causative agents of disseminated candidiasis are Candida species, with C. albicans being the most prevalent. Other species such as C. tropicalis, C. glabrata, and C. parapsilosis have also been implicated. Key risk factors include:
- Immunosuppression: Patients with hematologic malignancies, HIV/AIDS, or those on immunosuppressive therapies are highly susceptible.
- Prolonged Neutropenia: Extended periods of low neutrophil counts, often due to chemotherapy, increase the risk.
- Broad-Spectrum Antibiotic Use: Disruption of normal flora can facilitate fungal overgrowth.
- Invasive Medical Devices: Central venous catheters and other indwelling devices can serve as entry points for Candida.
- ICU Admission: Critical illness and associated interventions elevate the risk of infection.
Pathophysiology
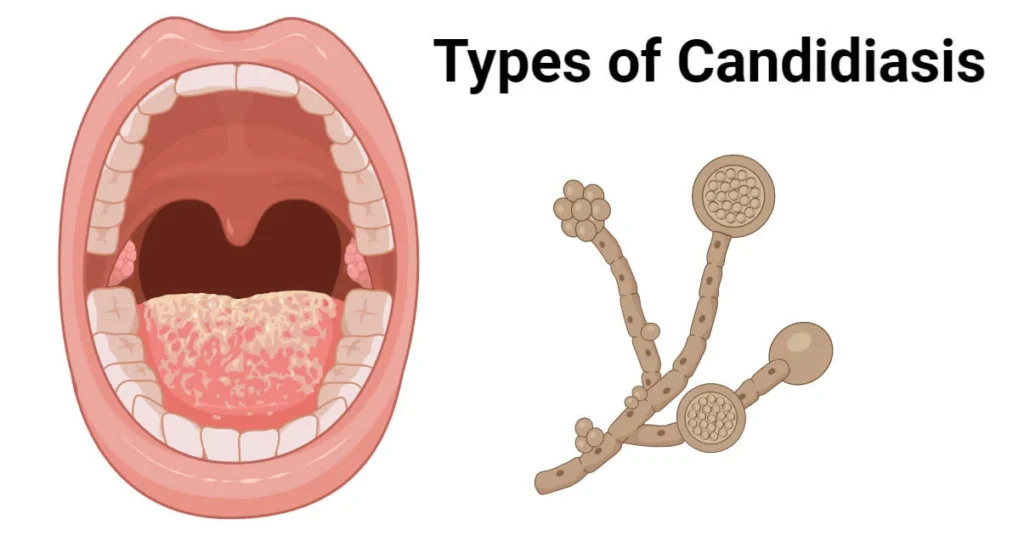
Candida species are commensal organisms residing on mucosal surfaces. Under certain conditions, they can translocate across epithelial barriers into the bloodstream, leading to hematogenous dissemination. The pathogenicity of Candida involves:
- Adhesion: Ability to adhere to host tissues and medical devices.
- Biofilm Formation: Development of structured communities that enhance resistance to antifungal agents.
- Morphological Transition: Switching from yeast to hyphal forms facilitates tissue invasion.
Clinical Manifestations
Disseminated candidiasis presents with a spectrum of symptoms, often nonspecific, making early diagnosis challenging. Common manifestations include:
- Persistent Fever: Unresponsive to broad-spectrum antibiotics.
- Organ-Specific Symptoms: Depending on the organs involved, patients may exhibit signs of hepatosplenic involvement, renal abscesses, endophthalmitis, or skin lesions.
- Sepsis: In severe cases, systemic inflammatory response leading to septic shock.
Diagnostic Approaches
Accurate and timely diagnosis is crucial for effective management. Diagnostic modalities encompass:
- Blood Cultures: Standard method but may yield false negatives due to intermittent fungemia.
- Imaging Studies: CT or MRI scans to detect organ involvement such as abscesses.
- Histopathological Examination: Tissue biopsies revealing yeast and hyphal forms.
- Serological Tests: Detection of Candida antigens or antibodies, though specificity varies.
Treatment Strategies
Management of disseminated candidiasis involves prompt initiation of antifungal therapy and addressing underlying risk factors. Treatment options include:
- Echinocandins: First-line agents (e.g., caspofungin, micafungin) due to their efficacy and safety profile.
- Azoles: Fluconazole is effective, especially in less critically ill patients or as step-down therapy.
- Amphotericin B: Reserved for refractory cases or when resistance is suspected.
- Combination Therapy: May be considered in severe infections or when initial monotherapy fails.
Adjunctive Measures
- Source Control: Removal of infected devices or drainage of abscesses.
- Immune Modulation: In cases complicated by immune reconstitution inflammatory syndrome (IRIS), corticosteroids may be beneficial, as evidenced in pediatric patients with acute lymphocytic leukemia developing chronic disseminated candidiasis complicated by IRIS. pmc.ncbi.nlm.nih.gov
Prognosis
The outcome depends on several factors, including the patient’s underlying condition, timeliness of diagnosis, and initiation of appropriate therapy. Mortality rates remain high, underscoring the need for heightened clinical awareness and early intervention.
Prevention
Preventive strategies focus on minimizing risk factors:
- Antimicrobial Stewardship: Judicious use of antibiotics to prevent disruption of normal flora.
- Aseptic Techniques: Strict adherence to infection control practices during invasive procedures.
- Prophylactic Antifungals: In high-risk populations, prophylaxis may reduce the incidence of disseminated candidiasis.

