Diarrhea predominant irritable bowel syndrome is a functional gastrointestinal disorder characterized by a combination of chronic symptoms, including abdominal pain, bloating, and altered bowel habits. Among its subtypes, diarrhea-predominant IBS (IBS-D) is distinguished by frequent loose or watery stools. This article delves into the intricacies of IBS-D, encompassing its causes, symptoms, diagnostic criteria, and available treatment modalities.
Understanding IBS-D
IBS-D is identified by recurrent abdominal discomfort or pain associated with frequent episodes of diarrhea. The Rome IV criteria, a standardized tool for diagnosing functional gastrointestinal disorders, define IBS-D as abdominal pain occurring, on average, at least one day per week in the last three months, accompanied by two or more of the following:
- Pain related to defecation
- Change in stool frequency
- Change in stool form (appearance)
Additionally, for IBS-D classification, more than 25% of bowel movements should be loose or watery, and less than 25% should be hard or lumpy.
Etiology and Pathophysiology
The exact cause of IBS-D remains elusive; however, several factors are believed to contribute to its development:
- Gut-Brain Axis Dysregulation: Abnormal communication between the central nervous system and the gastrointestinal tract can lead to altered gut motility and heightened pain sensitivity.
- Intestinal Inflammation: Low-grade inflammation and increased intestinal permeability have been observed in IBS-D patients, suggesting an immune system involvement. gut.bmj.com
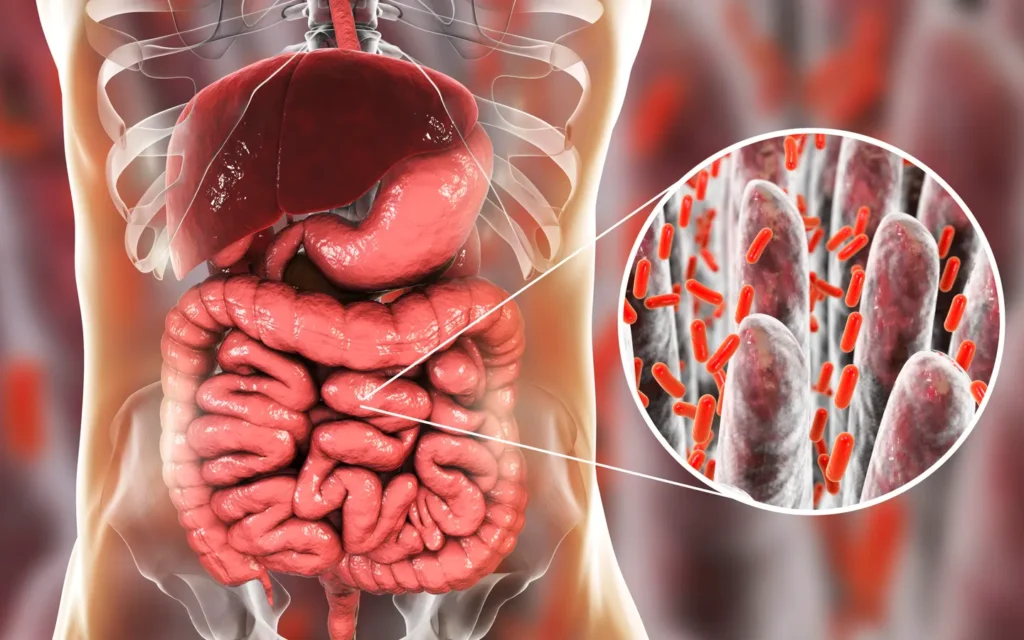
- Altered Gut Microbiota: An imbalance in the intestinal microbiome may disrupt normal digestive processes, contributing to symptoms.
- Post-Infectious Changes: A history of acute gastroenteritis can precede the onset of IBS-D, indicating that infections may trigger long-term changes in gut function.
Clinical Manifestations
Patients with IBS-D commonly experience:
- Frequent loose or watery stools
- Urgency to defecate
- Abdominal cramping and pain
- Bloating and gas
- Mucus in the stool
These symptoms can significantly impact daily activities and quality of life.
Diagnostic Approach
Diagnosing IBS-D involves a comprehensive evaluation:
- Medical History: Detailed assessment of symptom patterns, duration, and triggers.
- Physical Examination: To identify any palpable abnormalities or tenderness.
- Laboratory Tests: Including blood tests to rule out anemia or infection, and stool tests to exclude parasitic infections.
- Imaging Studies: Such as colonoscopy or flexible sigmoidoscopy to exclude structural abnormalities.
- Exclusion of Other Conditions: It’s crucial to differentiate IBS-D from other disorders like celiac disease, inflammatory bowel disease, and microscopic colitis.
Management Strategies
Treatment of IBS-D is multifaceted, aiming to alleviate symptoms and improve quality of life:
- Dietary Modifications:
- Low FODMAP Diet: Reducing intake of fermentable oligosaccharides, disaccharides, monosaccharides, and polyols can decrease bloating and diarrhea.
- Fiber Supplementation: Soluble fiber may help regulate bowel movements.
- Pharmacological Interventions:
- Antidiarrheal Agents: Loperamide can reduce stool frequency and urgency.
- Antispasmodics: Medications like hyoscyamine or dicyclomine may alleviate abdominal cramping.
- Bile Acid Sequestrants: For patients with bile acid malabsorption, agents like cholestyramine can be beneficial.
- Serotonin Receptor Antagonists: Alosetron is approved for women with severe IBS-D unresponsive to other treatments.
- Antibiotics: Rifaximin has shown efficacy in reducing symptoms, possibly by altering gut microbiota.
- Eluxadoline: A mixed opioid receptor modulator that can decrease bowel contractions and reduce diarrhea.
- Psychological Therapies:
- Cognitive Behavioral Therapy (CBT): Addresses the psychological aspects contributing to symptom perception.
- Gut-Directed Hypnotherapy: Has been shown to reduce IBS symptoms in some patients.
MYHEALTHMAG