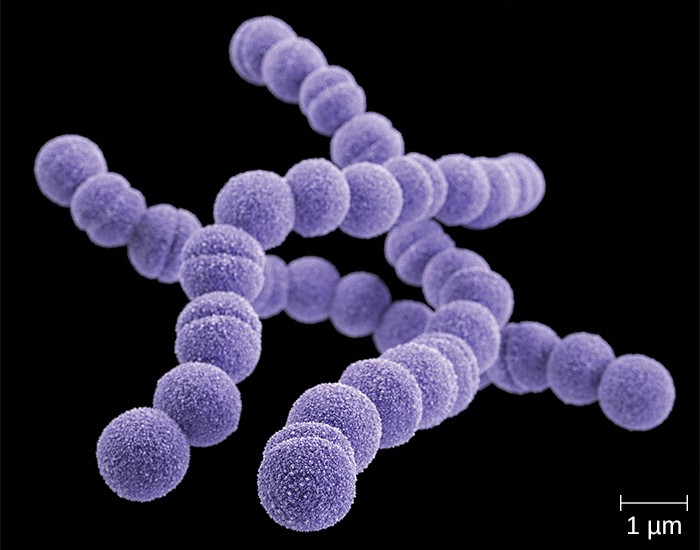
Acute Streptococcus pyogenes bacterial sinusitis is a severe infection of the paranasal sinuses caused by S. pyogenes, a Group A streptococcus (GAS). Although viral infections account for most sinusitis cases, bacterial infections, particularly those caused by S. pyogenes, lead to prolonged symptoms, complications, and require targeted antibiotic therapy.
Pathophysiology of S. pyogenes in Sinus Infections
S. pyogenes invades the upper respiratory tract, triggering an inflammatory response in the sinuses. This results in increased mucus production, swelling of the mucosa, and obstruction of normal sinus drainage, leading to infection progression.
Causes and Risk Factors
Factors that predispose individuals to acute S. pyogenes sinusitis include:
- Recent Upper Respiratory Infections (URIs): Viral infections weaken the mucosal barrier.
- Allergic Rhinitis: Chronic inflammation increases susceptibility.
- Nasal Obstruction: Deviated septum or polyps impede drainage.
- Immunocompromised State: Diabetes, HIV, or chemotherapy patients have higher risk.
- Exposure to Pathogens: Close contact with infected individuals.
Clinical Symptoms
The hallmark signs of acute S. pyogenes bacterial sinusitis include:
- Severe Nasal Congestion: Persistent blockage and difficulty breathing.
- Purulent Nasal Discharge: Thick yellow or green mucus.
- Facial Pain and Pressure: Especially in the forehead, cheeks, or around the eyes.
- Fever: Often higher than in viral sinusitis cases.
- Postnasal Drip and Sore Throat: Due to mucus draining into the throat.
- Headache and Fatigue: Resulting from systemic inflammation.
Diagnosis
Accurate diagnosis is essential for effective treatment. Key diagnostic steps include:
- Clinical Examination: Evaluation of sinus tenderness, nasal discharge, and systemic symptoms.
- Nasopharyngeal Swab and Culture: Identifies S. pyogenes as the causative agent.
- Blood Tests: Elevated white blood cell count and C-reactive protein (CRP) levels indicate bacterial infection.
- Imaging Studies: CT scans help detect sinus opacification and structural abnormalities.
Treatment Options
1. Antibiotic Therapy
- First-line treatment: Penicillin or amoxicillin-clavulanate.
- Alternative antibiotics: Cephalosporins, macrolides (azithromycin, clarithromycin) for penicillin-allergic patients.
- Avoidance of broad-spectrum antibiotics: To minimize resistance development.
2. Symptomatic Relief
- Nasal Irrigation: Saline sprays help clear mucus.
- Decongestants: Pseudoephedrine reduces nasal swelling.
- Pain Management: Ibuprofen or acetaminophen alleviates facial pressure.
- Steam Inhalation: Opens blocked sinuses for better drainage.
3. Surgical Intervention (Severe or Recurrent Cases)
- Endoscopic Sinus Surgery (ESS): Removes obstructions and improves drainage.
- Balloon Sinuplasty: Minimally invasive procedure to widen sinus passages.
Prevention Strategies
- Hand Hygiene and Respiratory Etiquette: Reduces transmission risk.
- Avoidance of Smoking and Pollutants: Prevents mucosal damage.
- Vaccination: Influenza and pneumococcal vaccines help lower bacterial sinusitis risk.
- Prompt Treatment of Strep Throat: Prevents progression to sinusitis.
Potential Complications
Without proper management, acute S. pyogenes sinusitis can lead to:
- Orbital Cellulitis: Infection spreading to the eye socket.
- Sinus Thrombosis: Clot formation in sinus veins.
- Meningitis: Bacterial spread to the central nervous system.
- Chronic Sinusitis: Recurrent infections requiring long-term care.
Acute Streptococcus pyogenes bacterial sinusitis is a serious but treatable condition. Early diagnosis, appropriate antibiotics, and preventive measures are crucial for effective management and improved patient outcomes.