Acquired thrombotic thrombocytopenic purpura (aTTP) is a rare but life-threatening hematological disorder characterized by microvascular thrombosis, low platelet counts, and organ ischemia. Early diagnosis and treatment are essential to prevent severe complications and improve survival rates. This guide provides an in-depth overview of aTTP, including its causes, symptoms, diagnostic methods, and treatment options.
Understanding Acquired Thrombotic Thrombocytopenic Purpura (aTTP)
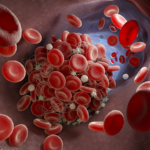
aTTP is an autoimmune condition where autoantibodies inhibit ADAMTS13, a metalloprotease enzyme responsible for cleaving von Willebrand factor (vWF). This inhibition leads to the accumulation of large vWF multimers, causing widespread platelet aggregation and microvascular occlusions.
Key Characteristics of aTTP
- Thrombocytopenia: Low platelet count due to consumption in thrombus formation.
- Microangiopathic Hemolytic Anemia (MAHA): Red blood cell destruction as they pass through narrowed blood vessels.
- Organ Dysfunction: Ischemic damage to organs, such as the brain, heart, and kidneys.
Causes and Risk Factors of aTTP
aTTP is primarily an autoimmune disorder. The exact cause of the immune dysregulation remains unknown, but several risk factors have been identified:
- Autoimmune Conditions: Diseases such as lupus or rheumatoid arthritis can predispose individuals to aTTP.
- Infections: Certain viral and bacterial infections may trigger autoantibody production.
- Pregnancy: Hormonal changes and immune system modulation during pregnancy increase the risk.
- Medications: Drugs like quinine, clopidogrel, and cyclosporine are associated with aTTP in some cases.
- Cancer: Hematologic malignancies can exacerbate autoimmune dysfunction.
Symptoms of Acquired Thrombotic Thrombocytopenic Purpura
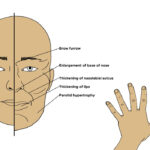
The presentation of aTTP varies, but common symptoms include:
- Fatigue and weakness due to anemia.
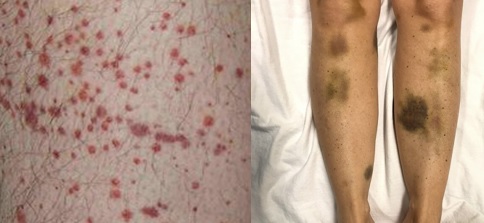
- Petechiae or purpura caused by thrombocytopenia.
- Neurological symptoms such as confusion, seizures, or stroke.
- Abdominal pain and nausea from gastrointestinal involvement.
- Chest pain or dyspnea indicating cardiac ischemia.
The “Pentad” of Classic Symptoms
The classic pentad of symptoms includes:
- Thrombocytopenia.
- MAHA.
- Neurological deficits.
- Renal impairment.
- Fever.
Although rare, this pentad helps in clinical diagnosis.
Diagnosis of aTTP
Timely diagnosis of aTTP is critical to prevent mortality. The following diagnostic methods are commonly employed:
1. Blood Tests
- Complete Blood Count (CBC): Reveals thrombocytopenia and anemia.
- Peripheral Blood Smear: Shows schistocytes, confirming MAHA.
- LDH and Bilirubin: Elevated levels indicate hemolysis.
2. ADAMTS13 Activity Assay
- Measures the activity of ADAMTS13 enzyme.
- Levels <10% confirm severe deficiency, suggestive of aTTP.
3. Autoantibody Testing
- Detects inhibitory antibodies against ADAMTS13.
4. Other Diagnostic Tools
- Coagulation Tests: Differentiate aTTP from disseminated intravascular coagulation (DIC).
- Imaging Studies: Assess organ ischemia or infarctions.
Treatment Options for aTTP
Early and aggressive treatment is essential to prevent fatal outcomes in aTTP. Therapeutic strategies include:
1. Plasma Exchange Therapy (PEX)
PEX is the cornerstone of aTTP treatment. It removes autoantibodies and replenishes ADAMTS13 levels. Daily sessions are initiated immediately after diagnosis and continued until platelet counts normalize.
2. Corticosteroids
High-dose corticosteroids are used to suppress the immune system and reduce antibody production.
3. Rituximab
Rituximab, a monoclonal antibody targeting CD20, is often administered in refractory or relapsing cases to eliminate B cells producing autoantibodies.
4. Caplacizumab
This anti-vWF nanobody inhibits platelet aggregation, preventing thrombus formation. It is used alongside PEX and corticosteroids for rapid symptom resolution.
5. Supportive Care
- Red Blood Cell Transfusions: To address severe anemia.
- Dialysis: For patients with renal failure.
- Antiplatelet Therapy: To reduce thrombotic complications in specific cases.
Long-Term Management and Monitoring
Preventing Relapse
- Regular monitoring of ADAMTS13 activity helps identify patients at risk of relapse.
- Maintenance therapy with rituximab or other immunosuppressants may be required for recurrent cases.
Patient Education
Educating patients about the importance of follow-up visits, recognizing early symptoms, and maintaining a healthy lifestyle is essential to prevent complications.
Acquired thrombotic thrombocytopenic purpura is a medical emergency requiring prompt recognition and treatment. With advancements in therapeutic options like PEX, corticosteroids, and targeted therapies such as caplacizumab, the prognosis for patients with aTTP has improved significantly. Ongoing research continues to provide insights into better understanding and managing this complex disorder, ensuring improved outcomes for patients worldwide.