Bladder cancer is one of the most common malignancies worldwide, necessitating early and accurate detection to improve prognosis and treatment outcomes. Among the various diagnostic methods, cystoscopy remains the gold standard for visualizing and identifying bladder tumors. However, in patients with severe insulin resistance, diagnostic challenges arise, making cystoscopy even more essential. This article delves into the significance of cystoscopy in bladder cancer detection, particularly in individuals with metabolic disorders.
Understanding Diagnostic Cystoscopy
Diagnostic cystoscopy is a minimally invasive procedure that allows direct visualization of the bladder lining to detect abnormalities, including tumors, inflammation, and structural changes. The procedure involves inserting a cystoscope—a thin, flexible or rigid tube equipped with a camera—through the urethra into the bladder. It provides real-time imaging, enabling physicians to detect early-stage cancer lesions that may not be visible on other diagnostic tests like ultrasound or CT scans.
Types of Cystoscopy
- Flexible Cystoscopy: Performed under local anesthesia; commonly used for diagnostic purposes and routine surveillance.
- Rigid Cystoscopy: Requires general or spinal anesthesia; preferred for biopsy collection and surgical interventions.
Both methods are crucial in identifying bladder tumors, but the choice of technique depends on patient factors and clinical indications.
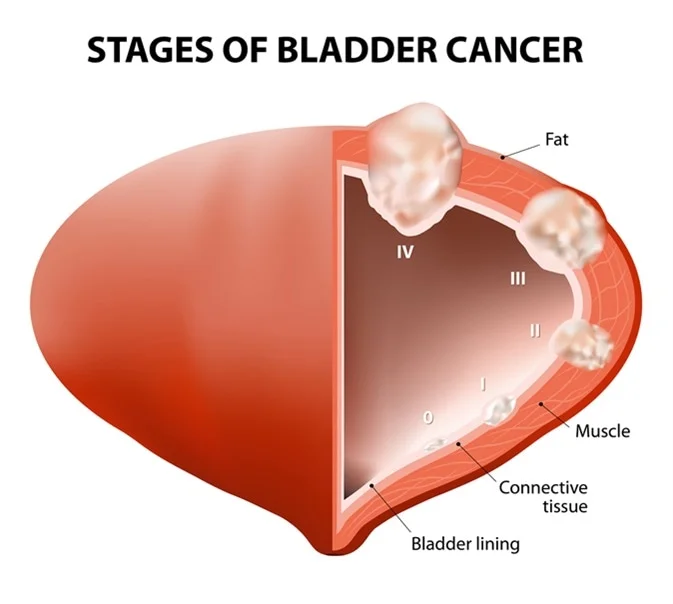
Bladder Cancer Detection via Cystoscopy
Cystoscopy plays a critical role in diagnosing bladder cancer, especially non-muscle invasive bladder cancer (NMIBC), which comprises the majority of bladder cancer cases. The procedure enables:
- Direct visualization of tumors: Unlike imaging techniques, cystoscopy allows real-time inspection of the bladder lining.
- Biopsy collection: Suspicious lesions can be sampled for histopathological examination to confirm malignancy.
- Tumor grading and staging: Helps differentiate between superficial and invasive tumors.
- Surveillance post-treatment: Essential for monitoring recurrence in patients with a history of bladder cancer.
Given its high sensitivity and specificity, cystoscopy remains the frontline tool for detecting urothelial carcinoma.
Severe Insulin Resistance and Its Impact on Bladder Cancer Diagnosis
Severe insulin resistance, commonly associated with metabolic syndrome, obesity, and type 2 diabetes, has been linked to an increased risk of malignancies, including bladder cancer. The interplay between insulin resistance and carcinogenesis involves multiple mechanisms, such as:
- Hyperinsulinemia: Promotes cell proliferation and inhibits apoptosis, potentially accelerating tumor growth.
- Chronic inflammation: Elevated levels of inflammatory cytokines contribute to DNA damage and tumor progression.
- Oxidative stress: Increases susceptibility to genetic mutations leading to malignancies.
- Metabolic dysregulation: Alters cellular signaling pathways, influencing cancer development and progression.
Patients with severe insulin resistance often experience delayed bladder cancer diagnosis due to overlapping symptoms, such as frequent urination and nocturia, which are also common in metabolic disorders. Therefore, cystoscopic evaluation is crucial in these high-risk individuals to ensure timely detection.
Benefits of Cystoscopy in Insulin-Resistant Patients
In patients with severe insulin resistance, cystoscopy offers several advantages in bladder cancer diagnosis and management:
1. Early Detection of Cancerous Lesions
Cystoscopy allows direct inspection of the bladder mucosa, identifying suspicious lesions at an early stage when they are most treatable.
2. Accurate Biopsy and Pathological Analysis
Tissue samples collected during cystoscopy enable precise histological assessment, differentiating between benign and malignant growths.
3. Minimally Invasive and Highly Effective
Compared to other diagnostic modalities, cystoscopy is a straightforward and minimally invasive procedure with high diagnostic yield.
4. Integration with Advanced Techniques
Cystoscopy can be combined with fluorescence cystoscopy (blue-light cystoscopy) or narrow-band imaging (NBI) to enhance tumor detection, particularly in high-risk patients.
Procedure Overview: What to Expect During Cystoscopy
Pre-Procedure Preparation
- Patients may need to provide a urine sample to rule out infections before the procedure.
- Local or general anesthesia is administered based on the type of cystoscopy performed.
- The bladder is filled with sterile fluid to expand it for better visualization.
Step-by-Step Cystoscopy Process
- Insertion of Cystoscope: The device is carefully guided through the urethra into the bladder.
- Bladder Examination: The physician inspects the bladder walls for tumors, lesions, or inflammation.
- Biopsy Collection (if needed): If abnormalities are detected, small tissue samples are taken.
- Completion and Recovery: The procedure lasts 10-20 minutes, and patients can resume normal activities shortly afterward.
Potential Risks and Considerations
While cystoscopy is generally safe, certain risks and precautions should be noted, particularly in insulin-resistant patients:
- Increased Infection Risk: Insulin resistance is associated with impaired immune function, raising susceptibility to urinary tract infections (UTIs). Preventative antibiotics may be prescribed.
- Delayed Healing: Wound healing may be slower in diabetic patients, necessitating close post-procedure monitoring.
- Bladder Irritation and Hematuria: Temporary discomfort, burning sensation, and minor bleeding are common but usually resolve within a few days.
Future Perspectives: Enhancing Bladder Cancer Detection in High-Risk Groups
Advancements in cystoscopic technology continue to improve diagnostic accuracy, particularly in insulin-resistant patients. Emerging techniques such as:
- Optical coherence tomography (OCT): Provides high-resolution imaging of bladder tissues.
- Molecular urine markers: Complement cystoscopy by detecting cancer-related biomarkers.
- Artificial intelligence-assisted cystoscopy: Enhances real-time image analysis for more precise tumor detection.
Integrating these innovations with traditional cystoscopy will further optimize bladder cancer diagnosis, especially in individuals with metabolic disorders.